University certificate
The world's largest faculty of medicine”
Why study at TECH?
With TECH, you will master the latest criteria related to Speech Therapy Neurorehabilitation and Vital Functions Analysis through an educational modality that integrates with excellence the theoretical and practical aspects of this discipline"

In very few years, science and technology have advanced considerably, leading to the emergence of effective protocols for Speech Neurorehabilitation and Vital Function Analysis. Likewise, orofacial and myofunctional therapies have been expanded for the care of patients with pathologies such as Aphasia and Hypophonia generated by Parkinson's disease. However, staying up to date on all these topics is a major challenge for specialists. This is largely due to the fact that the educational programs on the market are not sufficiently comprehensive or up to date on all the clinical and technological aspects of this discipline.
TECH wants to distinguish itself in this educational panorama with an unusual proposal that brings together, in a pioneering way, theoretical and practical learning. Therefore, this Hybrid Professional Master's Degree consists, first of all, of an online phase of 1800 hours. During this pedagogical process, the specialist will assimilate new knowledge with the support of multimedia resources such as infographics and videos. Likewise, they will be assisted by innovative methodologies such as apprenticeship to acquire these new competencies in a fast and flexible way.
On the other hand, at the end of this theoretical stage, the professionals will have in their hands the realization of a clinical practice in state-of-the-art hospital centers. This intensive, on-site internship will be developed for 3 weeks in a direct and immersive manner. The care of real patients is guaranteed during this learning period. In addition, they will be guided by prestigious experts and a designated tutor will closely monitor their progress. Upon completion of the entire program, the specialists will be ready to apply the latest techniques in their daily professional practice.
Through this Hybrid Professional Master's Degree you will be able to apply specific relaxation techniques for the tone and voluntary motor control of patients with Facial Paralysis"
This Hybrid professional master’s degree in Speech Neurorehabilitation and Vital Function Analysis. Orofacial and Myofunctional Therapy contains the most complete and up-to-date scientific program on the market.The most important features include:
- Development of more than 100 clinical cases presented by health professionals with a wide experience in Speech-Language Neurorehabilitation and Vital Functions Analysis
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- Comprehensive systematized action plans for the main pathologies
- Presentation of practical workshops on diagnostic and therapeutic techniques Interactive learning system based on algorithms for decision making on clinical situations
- Practical clinical guides on approaching different pathologies
- All of this will be complemented by theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
- Furthermore, you will be able to carry out a clinical internship in one of the best hospital centers
You will apply the most innovative procedures of Speech Neurorehabilitation and Vital Functions Analysis during the 3 weeks of intensive practical internship offered by TECHH"
In this Hybrid professional master’s degree, with a vocational nature and blended learning modality, the program is aimed at updating healthcare professionals who require a high level of qualification. The contents are based on the latest scientific evidence, and oriented in an educational way to integrate theoretical knowledge into practice, and the theoretical-practical elements will facilitate knowledge update and decision-making in patient management.
Thanks to its multimedia content developed with the latest educational technology, they will allow the health professional to learn in a contextual and situated learning environment, i.e., a simulated environment that will provide immersive learning programmed to train in real situations. This program is designed around Problem-Based Learning, whereby the physician must try to solve the different professional practice situations that arise during the course. For this purpose, the students will be assisted by an innovative interactive video system created by renowned and experienced experts.
With this program you will be up to date on the proper breathing, swallowing, chewing and phonation patterns, as well as the proper positioning of the lips and tongue, according to specific alterations"

From this program, you will update your knowledge on how to train patients to prevent the hypophonia typical of Parkinson's disease"
Teaching Planning
The syllabus of this program is made up of a large number of modules and topics of educational interest. It includes the basic fundamentals of the Speech Neurorehabilitation, Vital Functions Analysis and Orofacial and Myofunctional Therapies. It also refers to the main developments in this field, providing professionals with a complete update. The entire syllabus is supported by innovative teaching methodologies, such as Relearning, and multimedia resources, such as videos, infographics and multimedia summaries. Through them, the graduates will be able to assimilate contents and incorporate them into their practice in a more efficient way.

100% online and free of pre-established study schedules: this is the first stage of TECH's excellent educational program"
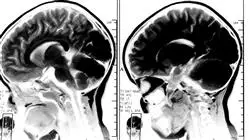
Module 1. Introduction to Neurorehabilitation I: Fundamentals of Neuroanatomy
1.1. History of Brain Discovery
1.1.1. Introduction
1.1.2. Stages in Brain History: Mind vs. Brain
1.1.2.1. From Antiquity to the 2nd Century
1.1.2.2. From the 2nd to the 17th Century
1.1.2.3. From the 19th Century to the Present
1.1.3. A Modern Vision of the Brain
1.1.4. Neuropsychological Rehabilitation
1.1.5. Conclusions
1.1.6. Bibliography
1.2. Introduction to the Nervous System
1.2.1. Introduction
1.2.2. Neurons
1.2.2.1. Cell Anatomy
1.2.2.2. Cell Functions
1.2.2.3. Classification of Neurons
1.2.2.4. Support Cells or Glia
1.2.3. Transmitting Information
1.2.3.1. Action Potentials
1.2.3.1.1. Resting Potential
1.2.3.1.2. Action Potential
1.2.3.1.3. Postsynaptic Potential, Local or Graded
1.2.4. Neuronal Circuits
1.2.5. Hierarchical Neural Organization
1.2.5.1. Introduction
1.2.5.2. Features
1.2.6. Brain Plasticity
1.2.7. Conclusions
1.3. Neurodevelopment
1.3.1. Introduction
1.3.2. Phases in Brain Development
1.3.2.1. Neurogenesis: Proliferation
1.3.2.2. Cell Migration
1.3.2.3. Cell Differentiation
1.3.2.4. Synaptogenesis
1.3.2.5. Apoptosis: Neuronal Death
1.3.2.6. Myelenization
1.3.3. Brain Maturation from Birth to Adolescence
1.3.4. Actuation Systems in Newborns: Reflexes
1.3.5. Warning Signs
1.3.6. Conclusions
1.3.7. Bibliography
1.4. Central Nervous System
1.4.1. Introduction
1.4.2. Peripheral Nervous System
1.4.3. Central Nervous System
1.4.3.1. CNS Protection System: Meninges
1.4.3.2. Irrigation of the CNS
1.4.3.3. Spinal Cord
1.4.3.4. Brain
1.4.3.4.1. Introduction
1.4.3.4.2. Structure
1.4.3.4.2.1. Brain Stem
1.4.3.4.2.2. Rhombencephalon or Hindbrain
1.4.3.4.2.3. Mesencephalon or Midbrain
1.4.3.4.2.4. Prosencephalon or Forebrain
1.4.4. Conclusions
1.4.5. Bibliography
1.5. Structural and Functional Organization of the Cerebral Cortex
1.5.1. Introduction
1.5.2. Brodmann Map
1.5.3. Cerebral Hemispheres and Cerebral Cortex: Structural Organization
1.5.3.1. Circumvolutions and Main Sulci: Cerebral Lobes
1.5.3.2. Structure of the Cerebral Cortex
1.5.3.3. White Matter
1.5.3.3.1. Association Fibers
1.5.3.3.2. Commissural Fibers
1.5.3.3.3. Projection Fibers
1.5.4. Cortical Areas: Functional Organization
1.5.5. Conclusions
1.5.6. Bibliography
1.6. Spinal Cord Pathways
1.6.1. Spinal Cord
1.6.2. Ascending Cord Pathways
1.6.3. Anatomical Organization
1.6.4. Functions and Lesions of the Ascending Pathways
1.6.5. Descending Cord Pathways
1.6.6. Anatomical Organization
1.6.7. Descending Tract Functions
1.6.8. Descending Tract Lesions
1.6.9. Sensory Receptors
1.6.10. Anatomical Types of Receptors
1.7. Cranial Nerves
1.7.1. Basic Vocabulary
1.7.2. History
1.7.3. Introduction
1.7.4. Nerve Components
1.7.5. Classification of Cranial Nerves
1.7.6. Pathologies
1.7.7. Summary
1.8. Spinal nerves
1.8.1. Introduction
1.8.2. Components
1.8.3. Dermatomes
1.8.4. Plexus
1.8.5. Cervical Plexus
1.8.6. Brachial Plexus
1.8.7. Lumbar Plexus
1.8.8. Sacral Plexus
1.8.9. Pathologies
1.9. Autonomic Nervous System
1.9.1. Basic Vocabulary
1.9.2. General Aspects
1.9.3. ANS Functions
1.9.4. Somatic Nervous System vs. Autonomous Nervous System
1.9.5. Organisation
1.9.6. Sympathetic ANS
1.9.7. Parasympathetic ANS
1.9.8. Enteric Nervous System
1.9.9. ANS Disorders
1.10. Motor Control
1.10.1. Somatosensory System
1.10.2. Upper Motor Circuit
1.10.3. Movement
1.10.4. Introduction to Motor Control
1.10.5. Clinical Applications of Motor Control and Learning in Neurorehabilitation
1.10.6. Neurological Impairment
1.10.7. Global Summary
Module 2. Introduction to Neurorehabilitation II: Speech Therapy Treatment
2.1. Etiology of Brain Damage
2.1.1. Introduction
2.1.2. Vascular Disorders
2.1.2.1. Occlusive Syndromes
2.1.2.2. Types of Cerebrovascular Disease
2.1.2.3. Neuropsychological Disorders in CVA
2.1.3. Intracranial Neoplasms
2.1.3.1. General Characteristics
2.1.3.2. Tumor Classification
2.1.3.3. Neuropsychological Disorders in Tumours
2.1.4. Cranioencephalic Trauma (CET)
2.1.4.1. General Characteristics
2.1.4.2. Types of CET
2.1.4.3. CET Disorders
2.1.5. Neurodegenerative Diseases
2.1.5.1. General Characteristics
2.1.5.2. Types and Disorders
2.1.6. Epilepsy
2.1.6.1. General Characteristics
2.1.6.2. Classification
2.1.7. Central Nervous System Infections.
2.1.7.1. General Characteristics
2.1.7.2. Classification
2.1.8. Cerebrospinal Fluid Circulation and Disorders
2.1.8.1. General Characteristics
2.1.8.2. Disorders
2.1.9. Global Summary
2.2. Cognitive Functions I: Attention, Perception and Memory
2.2.1. Introduction to Cognitive Functions
2.2.2. Alertness System
2.2.2.1. Concept
2.2.2.2. Assessment
2.2.2.3. Abnormalities
2.2.3. Attention
2.2.3.1. Focused/Selective Attention
2.2.3.1.1. Concept
2.2.3.1.2. Assessment
2.2.3.1.3. Abnormalities
2.2.3.2. Sustained Attention
2.2.3.2.1. Concept
2.2.3.2.2. Assessment
2.2.3.2.3. Abnormalities
2.2.3.3. Alternating Attention
2.2.3.3.1. Concept
2.2.3.3.2. Assessment
2.2.3.3.3. Abnormalities
2.2.3.4. Divided attention
2.2.3.4.1. Concept
2.2.3.4.2. Assessment
2.2.3.4.3. Abnormalities
2.2.4. Memory
2.2.4.1. Concept
2.2.4.2. Process
2.2.4.3. Classification
2.2.4.4. Assessment
2.2.4.5. Abnormalities
2.2.5. Perception
2.2.5.1. Concept
2.2.5.2. Assessment
2.2.5.3. Abnormalities
2.3. Cognitive Functions II: Language and Executive Functions
2.3.1. Conceptualization of Executive Functions
2.3.2. Executive Functions Assessment
2.3.3. Executive Function Disorders
2.3.4. Dorsolateral Prefrontal Syndrome
2.3.5. Orbitofrontal Syndrome
2.3.6. Mesial Frontal Syndrome
2.3.7. Conceptualization of Language
2.3.8. Language Evaluation
2.3.9. Language Impairment
2.4. Neuropsychological Assessment
2.4.1. Introduction
2.4.2. Neuropsychological Assessment Objectives
2.4.3. Assessment Variables
2.4.4. Diffuse vs. Local Brain Injury
2.4.5. Injury Location and Size
2.4.6. Injury Depth
2.4.7. Distant Effects of the Injury
2.4.8. Disconnection Syndrome
2.4.9. Injury Time Evolution
2.4.10. Intrinsic Patient-Related Variables
2.4.11. Quantitative vs. Qualitative Assessment
2.4.12. Stages in Neuropsychological Assessment
2.4.13. Clinical History and Establishing Therapeutic Relationships
2.4.14. Test Administration and Correction
2.4.15. Analyzing and Interpreting Results, Preparing Reports and Returning Information
2.5. Neuropsychological Rehabilitation and Speech Therapy Applications
2.5.1. Neuropsychological Rehabilitation I: Cognitive Functions
2.5.1.1. Introduction
2.5.2. Attention and Perception
2.5.2.1. Training Attention Processes
2.5.2.2. Effectiveness
2.5.2.3. Virtual reality
2.5.3. Memory
2.5.3.1. Basic Principles
2.5.3.2. Memory Strategies
2.5.3.3. Virtual reality
2.5.4. Apraxias
2.5.4.1. Stimulation Strategies
2.5.4.2. Specific Tasks
2.5.5. Language
2.5.5.1. General Advice
2.5.5.2. Specific Tasks
2.5.6. Executive Functions (EF)
2.5.6.1. General Advice
2.5.6.2. EF Stimulation
2.5.6.2.1. Sohlberg and Mateer
2.5.6.2.2. Executive Deficit Treatment Techniques
2.5.6.3. Specific Tasks
2.5.6.4. Effectiveness
2.5.7. Summary
2.5.8. Bibliography
2.6. Behavioural Rehabilitation and Speech Therapy Applications
2.6.1. Introduction
2.6.1.1. ERC Reference Model
2.6.1.2. Orientations/Currents
2.6.1.3. Behavior Modification Characteristics
2.6.1.4. Behavior Modification Techniques: General Use/Specific Use
2.6.2. Behavioral Assessment: Observation
2.6.2.1. Define Target Behavior
2.6.2.2. Choose Measurement Methods
2.6.2.3. Record Sheets
2.6.2.4. Contextual Aspects of What Is Observed
2.6.3. Operant Techniques: Behavioral Development
2.6.3.1. Introduction
2.6.3.2. Theoretical Concepts
2.6.3.3. Reinforcement Programs
2.6.3.4. Molding
2.6.3.5. Chaining
2.6.3.6. Fading
2.6.3.7. Negative Reinforcement
2.6.3.8. Scope of Application
2.6.4. Operant Techniques: Behavior Reduction
2.6.4.1. Introduction
2.6.4.2. Extinction
2.6.4.3. Time Off
2.6.4.4. Cost of Response
2.6.4.5. Scope of Application
2.6.5. Operant Techniques: Contingency Organization Systems
2.6.5.1. Introduction
2.6.5.2. Token Economy
2.6.5.3. Behavioral Contracts
2.6.5.4. Scope of Application
2.6.6. Modeling Techniques
2.6.6.1. Introduction
2.6.6.2. Procedure
2.6.6.3. Modeling Techniques
2.6.6.4. Scope of Application
2.6.7. Frequent Behavior in Logopedics
2.6.7.1. Impulsiveness
2.6.7.2. Apathy
2.6.7.3. Disinhibition
2.6.7.4. Anger or Aggressiveness
2.6.8. Conclusions
2.7. Rehabilitation in Occupational Therapy and Speech Therapy Applications
2.7.1. Occupational Therapy
2.7.2. Body Posture in Speech Therapy
2.7.3. Body Posture
2.7.4. Adaptations in Body Posture
2.7.5. Techniques in Neurorehabilitation: Bobath, Affolter, Basal Stimulation
2.7.6. Adaptations/Support Products Useful in Speech Therapy Rehabilitation
2.7.7. Objective of Occupational Therapy as an Integrative Measure
2.8. Child Neuropsychology
2.8.1. Introduction
2.8.2. Child Neuropsychology: Definition and General Foundation
2.8.3. Etiology
2.8.3.1. Genetic and Environmental Factors
2.8.3.2. Classification
2.8.3.2.1. Neurodevelopment Disorders
2.8.3.2.2. Acquired Brain Injury
2.8.4. Neuropsychological Assessment
2.8.4.1. General Aspects and Assessment Phase
2.8.4.2. Evaluation Tests
2.8.5. Neuropsychological Intervention
2.8.5.1. Family Intervention
2.8.5.2. Educational Intervention
2.8.6. Cognitive Function Development
2.8.6.1. First Childhood (0-2 Years of Age)
2.8.6.2. Preschool Period (2-6 Years of Age)
2.8.6.3. School Period (6-12 Years of Age)
2.8.6.4. Adolescence (12-20 Years of Age)
2.8.7. Conclusions
2.8.8. Bibliography
2.9. Family Approach and Therapy
2.9.1. Introduction
2.9.2. Family Care in the Acute and Subacute Phase
2.9.2.1. Acute Phase: Hospital Stay
2.9.2.2. Subacute Phase: Return Home
2.9.2.3. What about after Rehabilitation?
2.9.3. The Family as Part of the Rehabilitation Process
2.9.4. Needs Posed by the Family during the Rehabilitation Process
2.9.5. The Rehabilitation Team
2.9.6. Conclusions
2.9.7. Bibliography
2.10. A Transdisciplinary Rehabilitation Example: Clinical Case
2.10.1. Clinical Cases
2.10.2. CET Theories
2.10.3. Broca's Aphasia: Anatomopathological Correlates and Disorders Associated with Broca's Aphasia
2.10.4. Neuropsychological Assessment
2.10.5. Neuropsychological Profile
2.10.6. Results
2.10.7. Deficits and Potentials
2.10.8. Injury Course and Treatment
2.10.9. Specific Objectives for Patients with Broca's Aphasia
2.10.10. Fundamentals of Rehabilitation
Module 3. Anatomy and Physiology of the Voice
3.1. Voice Anatomy
3.1.1. Laryngeal Anatomy
3.1.2. Respiratory Structures Involved in Phonation
3.1.2.1. Chest
3.1.2.2. Airway
3.1.2.3. Respiratory Musculature
3.1.3. Laryngeal Structures Involved in Phonation
3.1.3.1. Laryngeal Skeleton
3.1.3.2. Cartilage
3.1.3.3. Joints
3.1.3.4. Musculature
3.1.3.5. Innervation
3.1.4. Structures of the Vocal Tract Involved in Phonation
3.1.4.1. Linear Source-Filter Model
3.1.4.2. Non-Linear Source-Filter Model
3.2. Voice Physiology
3.2.1. Histology of Vocal Folds
3.2.2. Biomechanical Properties of the Vocal Folds
3.2.3. Myoelastic Mucoondulatory Theory and Aerodynamic Theory
3.3. Pathological Voice
3.3.1. Euphonia vs Dysphonia
3.3.2. Vocal Fatigue
3.3.3. Acoustic Signs of Dysphonia
3.3.4. Classification of Dysphonia
3.4. Medical- Surgical Treatment
3.4.1. Phonosurgery
3.4.2. Laryngeal Surgery
3.4.3. Medication in Dysphonia
3.5. Physical and Acoustic Aspects
3.5.1. Physical Aspects of the Voice
3.5.1.1. Types of Waves
3.5.1.2. Physical Properties of Sound Waves: Amplitude and Frequency
3.5.1.3. Transmission of Sound
3.5.2. Acoustic Voice Aspects:
3.5.2.1. Intensity
3.5.2.2. Pitch
3.5.2.3. Quality
3.6. Objective Voice Assessment
3.6.1. Morphofunctional Exploration
3.6.2. Electroglottography
3.6.3. Aerodynamic Measures
3.6.4. Electromyography
3.6.5. Videochemography
3.6.6. Acoustic Analysis
3.7. Perceptual Assessment
3.7.1. GRBAS
3.7.2. RASAT
3.7.3. GBR Score
3.7.4. CAPE-V
3.7.5. VPAS
3.8. Functional Assessment
3.8.1. Fundamental Frequency
3.8.2. Phonetogram
3.8.3. Maximum Phonatory Times
3.8.4. Velo-Palatine Efficiency
3.8.5. VHI
3.9. Assessing Vocal Quality
3.9.1. Vocal Quality
3.9.2. High Quality Voice vs. Low Quality Voice
3.9.3. Vocal Quality Assessment in Voice Professionals
3.10. Medical History
3.10.1. The Importance of Medical History
3.10.2. Characteristics of the Initial Interview
3.10.3. Medical History Sections and Voice Implications
3.10.4. Proposal of a Model of Anamnesis for Vocal Pathology
Module 4. Vocal Rehabilitation
4.1. Speech Therapy Treatment for Functional Dysphonias
4.1.1. Type I: Isometric Laryngeal Disorder
4.1.2. Type II: Glottic and Supraglottic Lateral Contraction
4.1.3. Type III: Anteroposterior Supraglottic Contraction
4.1.4. Type IV: Conversion Aphonia/Dysphonia and Psychogenic Dysphonia with Arched Vocal Cords
4.1.5. Transitional Adolescent Dysphonia
4.2. Speech Therapy Treatment for Organic Dysphonia
4.2.1. Introduction
4.2.2. Speech Therapy in Congenital Origin Dysphonias
4.2.3. Speech Therapy in Acquired Origin Dysphonias
4.3. Speech Therapy Treatment for Organic-Functional Dysphonias
4.3.1. Introduction
4.3.2. Objectives in the Rehabilitation of Organic-Functional Pathologies
4.3.3. Proposal of Exercises and Techniques according to the Rehabilitation Objective
4.4. Voice in Acquired Neurological Problems
4.4.1. Dysphonias of Neurological Origin
4.4.2. Speech Therapy Treatment
4.5. Child Dysphonia
4.5.1. Anatomical Characteristics
4.5.2. Vocal Characteristics
4.5.3. Intervention
4.6. Hygiene Therapy
4.6.1. Introduction
4.6.2. Harmful Habits and Their Effect on the Voice
4.6.3. Preventive Measures
4.7. Semi-Occluded Vocal Tract Exercises
4.7.1. Introduction
4.7.2. Justification
4.7.3. TVSO
4.8. Estill Voice Training as a Technique to Improve Vocal Function
4.8.1. Jo Estill and the Creation of the Model
4.8.2. Principles of Estill Voice Training
4.8.3. Description
Module 5. Orofacial Myofunctional Therapy (OMT) and Early Care
5.1. Neonatal Development
5.1.1. Neonatal Development
5.1.2. NBAS: Neonatal Behavioral Assessment
5.1.3. Early Diagnosis.
5.1.4. Neurologic Diagnosis
5.1.5. Habituation
5.1.6. Oral Motor Reflexes
5.1.7. Body Reflexes
5.1.8. Vestibular System
5.1.9. Social and Interactive Media
5.1.10. Use of NBAS in High-Risk Newborns
5.2. Eating Disorders in Children
5.2.1. Feeding Processes
5.2.2. Pediatric Swallowing Physiology
5.2.3. Phases in Skill Acquisition
5.2.4. Deficits
5.2.5. Multidisciplinary Work
5.2.6. Warning Symptomatology
5.2.7. Premature Orofacial Development
5.2.8. Feeding Methods: Parenteral, Enteral, Tube, Gastrectomy, Oral (Modified or Unmodified Diet)
5.2.9. Gastroesophageal Reflux
5.3. Neurodevelopment and Infant diets
5.3.1. Embryonic Development
5.3.2. Appearance of Main Primary Functions
5.3.3. Risk Factors
5.3.4. Evolutionary Milestones
5.3.5. Synaptic Function
5.3.6. Immaturity
5.3.7. Neurological Maturity
5.4. Brain-Motor Skills
5.4.1. Innate Orofacial Motor Skills
5.4.2. Evolution of Orofacial Motor Patterns
5.4.3. Reflex Swallowing
5.4.4. Reflex Breathing
5.4.5. Reflex Suction
5.4.6. Assessing Infant Oral Reflexes
5.5. Nursing
5.5.1. Early Start
5.5.2. Impact at the Orofacial Level
5.5.3. Exclusivity
5.5.4. Optimal Nutrition
5.5.5. Spontaneous Maturation of Oral Musculature
5.5.6. Muscle Mobility and Synergy
5.5.7. Position
5.5.8. Therapeutic Recommendations
5.5.9. Intellectual Development
5.5.10. Intervention Program
5.6. Early Feeding Techniques
5.6.1. Newborn Feeding
5.6.2. Positioning Techniques
5.6.3. Signs of Good Positioning
5.6.4. Key Therapeutic Recommendations
5.6.5. Milk and Non-Milk Formulas
5.6.6. Classification of Formulas
5.6.7. Bottle Feeding Techniques
5.6.8. Spoon Techniques
5.6.9. Techniques for Low-Cut Cup Use
5.6.10. Techniques Tube Use or Alternative Feeding Systems
5.7. Speech Therapy Intervention in Neonates
5.7.1. Primary Functions Assessment
5.7.2. Re-Education of Primary Neuromotor Dysfunctions
5.7.3. Primary Intervention
5.7.4. Individual Treatment Planning and Coordination
5.7.5. Oral Motor Exercise Program I
5.7.6. Oral Motor Exercise Program II
5.7.7. Intervention with Families
5.7.8. Early Motor Activation
5.8. Child Swallowing Disorders: Block 1
5.8.1. Intake Analysis
5.8.2. Undernourishment
5.8.3. Respiratory Infections: Airway Unit
5.8.4. Complementary Explorations
5.8.5. Quantitative Explorations
5.8.6. Nutritional Treatment
5.8.7. Adaptive Treatment: Posture, Texture, Materials
5.8.8. Performance Program
5.9. Rehabilitative Treatment of Infant Oropharyngeal and Esophageal Dysphagia
5.9.1. Symptoms
5.9.2. Etiology
5.9.3. Neurological Damage in Children: High Probability of Presenting a Disorder
5.9.4. Infant Dysphagia
5.9.5. Phases of Normalized Swallowing in Pediatrics vs. Pathological Swallowing
5.9.6. Neurological Maturity: Cognitive, Emotional and Motor Coordination Status
5.9.7. Impossibility of Oral Feeding
5.9.8. Early care. High Probability of Recovering
5.10. Child Swallowing Disorders: Block 2
5.10.1. Types. Neuroanatomical and Behavior-Based Classification
5.10.2. Functional Maturational Dysphagia
5.10.3. Degenerative Diseases
5.10.4. Cardiorespiratory Pathologies
5.10.5. Congenital Brain Damage
5.10.6. Childhood Acquired Brain Injury (CABI)
5.10.7. Craniofacial Syndromes
5.10.8. Autism Spectrum Disorders
Module 6. Assessment and Intervention in Dysphagia of Neurological Origin in Adults
6.1. Swallowing: Definition and Anatomy
6.1.1. Definition of Swallowing
6.1.2. Swallowing Anatomy: Structures
6.1.2.1. Oral Cavity
6.1.2.2. Pharynx
6.1.2.3. Larynx.
6.1.2.4. Oesophageal
6.1.3. Swallowing Anatomy: Neurological Control
6.1.3.1. Central Nervous System
6.1.3.2. Cranial Nerves
6.1.3.3. Autonomic Nervous System
6.2. Swallowing: The Swallowing Process
6.2.1. Phases of Swallowing
6.2.1.1. Preoral Phase
6.2.1.2. Oral Phase
6.2.1.2.1. Oral Preparatory Phase
6.2.1.2.2. Oral Transport Phase
6.2.1.3. Pharyngeal Phase
6.2.1.4. Esophageal Phase
6.2.2. Valve System
6.2.3. Biomechanics of Swallowing
6.2.3.1. Swallowing Liquids
6.2.3.2. Swallowing Semi-Solids
6.2.3.3. Swallowing Solids: Chewing
6.2.4. Breathing-Swallowing Coordination
6.3. Introduction to Dysphagia
6.3.1. Definition
6.3.2. Etiology and Prevalence
6.3.2.1. Functional Causes
6.3.2.2. Organic Causes
6.3.3. Classification
6.3.3.1. Types of Dysphagia
6.3.3.2. Severity of Dysphagia
6.3.4. Structural vs. Neurogenic Dysphagia
6.3.5. Signs and Symptoms of Dysphagia
6.3.6. Safety and Efficacy Concepts
6.3.6.1. Safety Complications
6.3.6.2. Efficacy Complications
6.3.7. Brain Damage Dysphagia
6.3.8. Dysphagia in the Elderly
6.4. Medical Assessment of Dysphagia
6.4.1. Medical Anamnesis
6.4.2. Scales of Assessment and Screening
6.4.2.1. EAT-10
6.4.2.2. V-VST. Volume-Viscosity Swallow Test
6.4.2.2.1. How to Perform the V-VST
6.4.2.2.2. Useful Tips when Using V-VST
6.4.3. Instrumental Tests
6.4.3.1. Fibroendoscopy (FEES)
6.4.3.2. Videofluoroscopy (VFS)
6.4.3.3. Fibroendoscopy vs. Videofluoroscopy
6.4.3.4. Pharyngoesophageal Manometry
6.5. Speech Therapy Assessment of Dysphagia
6.5.1. Medical History
6.5.2. General Patient Assessment
6.5.2.1. Physical Examination
6.5.2.2. Cognitive Examination
6.5.3. Clinical Patient Exploration
6.5.3.1. Structural Assessment
6.5.3.2. Oral Motor and Sensory Examination
6.5.3.3. Cranial Nerves Assessment
6.5.3.4. Reflex Assessment
6.5.3.5. Exploring Swallowing by Phases (without Bolus)
6.5.3.6. Using Auscultation and Sound Assessment
6.5.3.7. Respiratory and Phonation Assessment
6.5.4. Tracheostomy Patient Assessment
6.5.5. Severity and Quality of Life Scales
6.6. Assessment of Nutritional Status
6.6.1. Importance of Nutrition
6.6.2. Screening Scales in Nutrition
6.6.2.1. Malnutrition Universal Screening Tool (MUST)
6.6.2.2. Mini Nutritional Assessment (MNA)
6.6.2.3. Nutritional Risk Screening 2002 (NRS 2002)
6.6.3. Nutritional Assessment
6.6.4. Undernourishment
6.6.5. Dehydration
6.6.6. Nutritional Supplements
6.6.7. Alternatives to Oral Feeding
6.6.7.1. Enteral Nutrition
6.6.7.1.1. Naso/Oroenteral Tube Nutrition
6.6.7.1.2. Nutrition by Gastrostomy
6.6.7.1.3. Comparing Types of Enteral Nutrition
6.6.7.2. Parenteral Nutrition
6.7. Dysphagia Rehabilitation Using Compensatory Techniques
6.7.1. Rehabilitation Treatment Objectives
6.7.2. Postural Techniques
6.7.3. Consistency Modifications
6.7.4. Modifying Intake Volume and Speed
6.7.5. Modifying Food at the Perceptual Level
6.7.6. New Textures
6.7.7. Adapting Utensils for Intake
6.7.8. Guidelines for Patients and Family
6.7.8.1. Adaptation to Surroundings
6.7.8.2. Drug Administration
6.7.8.3. Oral Hygiene
6.8. Dysphagia Rehabilitation Using Rehabilitation Techniques I
6.8.1. Inclusion/Exclusion Criteria in Treatments Using Rehabilitation Techniques
6.8.2. Swallowing Maneuvers
6.8.3. Techniques to Exercise Swallowing Musculature
6.8.3.1. Orofacial Myofunctional Therapy
6.8.3.1.1. Soft Tissues Manipulation
6.8.3.1.2. Sensory Enhancement Techniques
6.8.3.1.3. Specific Exercises
6.8.3.1.3.1. Tongue
6.8.3.1.3.2. Lips/Buccinator Muscles
6.8.3.1.3.3. Masticatory Muscles
6.8.3.1.3.4. Palatal Veil
6.8.3.2. Techniques to Stimulate Swallowing Reflex
6.8.3.3. Bolus Propulsion Exercises
6.8.3.4. Laryngeal Elevation (Hyoid Excursion) Exercises
6.8.3.5. Exercises to Improve Glottic Closure
6.9. Dysphagia Rehabilitation Using Rehabilitation Techniques II
6.9.1. Dysphagia Treatment based on Symptomatology
6.9.2. Breathing Treatment
6.9.3. Positioning
6.9.4. Diet Implementation
6.9.5. Use of Botulinum Toxin
6.9.6. Neuromuscular Bandaging
6.9.6.1. Rigid Bandages
6.9.6.2. Flexible Bandages
6.9.7. Electrotherapy in Swallowing
6.9.8. New Technologies
6.10. Useful Content for Speech Therapists Working in Dysphagia
6.10.1. CPR in Diet
6.10.2. Diet Rheology
6.10.3. Additional Information
Module 7. Dentistry and Orofacial Disorder
7.1. Dentition
7.1.1. Introduction
7.1.2. Tooth Growth and Development
7.1.3. Classification
7.1.4. Primary Dentition
7.1.5. Mixed Dentition
7.1.6. Permanent Dentition
7.1.7. Tooth Formation and Development
7.2. Normal/Typical and Pathological Pattern
7.2.1. Introduction
7.2.2. Apparatus
7.2.3. Dentolabial Deformities
7.2.4. Eruptive Abnormalities
7.2.5. Pathologic Patterns and Congenital Disorders
7.2.6. Clinical Assessment and Examination
7.2.7. Clinical Intervention
7.2.8. Multidisciplinary Perspective
7.3. Clinical Examination and Radiographic Analysis
7.3.1. Introduction
7.3.2. Overview
7.3.3. Teleradiography
7.3.4. Ricketts’ Circular Analysis
7.3.5. Steiner's Cephalometric Analysis
7.3.6. Bone Radiography
7.3.7. Bibliography
7.4. Assessment
7.4.1. Introduction
7.4.2. Orofacial System Functions
7.3.3. Aesthetic/Biofacial Analysis
7.3.4. Anatomical-Functional Assessment
7.3.5. Orofacial System Functions Assessment
7.3.6. Atypical Swallowing
7.3.7. Myofunctional Assessment Protocol
7.3.8. Bibliography
7.5. Function and Form
7.5.1. Introduction
7.5.2. Breathing and Swallowing Disorders
7.5.3. Breathing and Swallowing
7.5.4. Bruxism
7.5.5. Joint and Jaw Examination I
7.5.6. Joint and Jaw Examination I
7.5.7. Mandibular Dynamics Study
7.5.8. Bibliography
7.6. Speech Therapy Intervention
7.6.1. Introduction
7.6.2. Mouth Breathing
7.6.3. Oral Dysfunction
7.6.4. Speech Therapy Intervention in Oral Breathing
7.6.5. Atypical Swallowing
7.6.6. Speech Therapy Intervention in Atypical Swallowing
7.6.7. Temporomandibular Joint (TMJ)
7.6.8. Speech Therapy Intervention in TMJ
7.6.9. Bibliography
7.7. Occlusion and Malocclusion
7.7.1. Introduction
7.7.2. Temporal Occlusion
7.7.3. Temporal Occlusion Development
7.7.4. Permanent Occlusion
7.7.5. Permanent Occlusion Development
7.7.6. Physiological and Non-Physiological Occlusion
7.7.7. Static and Dynamic Occlusion
7.7.8. Multidisciplinary Treatment
7.7.9. Bibliography
7.8. Main Occlusion Classification
7.8.1. Introduction
7.8.2. Features
7.8.3. Anteroposterior Classification
7.8.4. Transversal Syndrome I
7.8.5. Transversal Syndrome II
7.8.6. Vertical Syndromes
7.8.7. Etiopathogenesis of Malocclusions
7.8.8. Bibliography
7.9. Dentistry and Speech Therapy
7.9.1. Introduction
7.9.2. Multidisciplinary Work
7.9.3. Extraoral Examination
7.9.4. Intraoral Examination
7.9.5. Functional Examination
7.9.6. Dentistry and Oral Function
7.9.7. Bibliography
7.9.8. Speech Therapy Intervention in Orofacial Disorder
7.10. Case Studies
7.10.1. Introduction
7.10.2. Case Study 1
7.10.3. Case Study 2
7.10.4. Case Study 3
7.10.5. Case Study 4
7.10.6. Bibliography
Module 8. Dietary Alteration in Congenital Neurological Disorder. PCI
8.1. Definition and History of ASD
8.1.1. Breathing
8.1.2. Respiratory Pattern and Classification
8.1.3. Airway Analysis
8.1.4. Chewing
8.1.5. Swallowing
8.1.6. Stomatognathic System Structures Involved in Swallowing
8.1.7. Neurological Structures Involved in Swallowing
8.1.8. Neurological Control of Swallowing
8.1.9. Neurogenic Dysphagia
8.1.10. Relation between Breathing and Swallowing: Importance of Breathing-Swallowing Coordination during Swallowing
8.2. Detection and Early Onset Diagnosis of Autism Spectrum Disorder
8.2.1. Neurological Disorders and Stomatognathic Development
8.2.2. Cranial Nerve Assessment
8.2.3. Oral Function Development
8.2.4. Facial Structure Growth
8.2.5. Orofacial System Disorders
8.2.6. Orofacial Maturation
8.2.7. Respiratory Structures
8.2.8. Facial Musculature
8.2.9. Oral Musculature
8.2.10. Laryngeal Musculature
8.3. Methodological Principles
8.3.1. Individualized Assessment for Diet Characteristics
8.3.2. Oral Reflexes Assessment
8.3.3. Diet and Cerebral Palsy, Main Associated Problems
8.3.4. Safety and Efficacy Disorders
8.3.5. Clinical Examination of Swallowing: What Tests Are Most Appropriate for People with CP?
8.3.6. Physical Examination - Gross Motor Function and Nutrition
8.3.7. Instrumental Examination
8.3.8. Which Diagnostic Test is the Most Effective for Diagnosing Dysphagia in People with CP?
8.3.9. Importance of Interdisciplinary Work in the Assessment of Dysphagia
8.3.9.1. How to Deal with the Assessment of Swallowing in People with CP?
8.3.9.2. When Should I Refer the Patient?
8.3.10. Procedure for Action in the Event of a Swallowing and/or Nutritional Problem
8.4. General Diet Intervention Guidelines
8.4.1. Definition
8.4.2. Main Characteristics
8.4.3. Speech Therapy Intervention and Treatment
8.4.4. Multidisciplinary Neurorehabilitation Treatment
8.4.5. Symptoms
8.4.6. Muscular Dysfunction
8.4.7. Active Control
8.4.8. Case Analysis
8.5. Dietary Problems in Children with ASD: Single Case Intervention Proposal. Part One
8.5.1. Definition
8.5.2. Main Characteristics
8.5.3. Speech Therapy Intervention and Treatment
8.5.4. Multidisciplinary Neurorehabilitation Treatment
8.5.5. Symptoms
8.5.6. Muscular Dysfunction
8.5.7. Active Control
8.5.8. Case Analysis
8.6. Dietary Problems in Children with ASD: Single Case Intervention Proposal. Part Two
8.6.1. First Phase: Postural, Oral and Nasal Hygiene
8.6.2. Implementing New Oral Habits
8.6.3. Creating Routines and Neuromotor Behaviors with High Frequency and Minimal Intensity
8.6.4. Second Phase: Intervention Program based on Structure Analysis
8.6.5. Creating Individualized Programs
8.6.6. Selecting Favorable Oral Motor Exercises
8.6.7. Third Phase: Feeding Strategies and Competences
8.6.8. Positioning
8.6.9. Developing Strategies for Adequate Oral Feeding
8.6.10. Enteral Feeding
8.7. Developing Strategies and Action Plans
8.7.1. Type of Diet
8.7.2. Texture and Consistency Adaptation
8.7.3. Volume Modification
8.7.4. Anticipation: Sensitive Strategies
8.7.5. Postural Adaptation Assessment
8.7.6. Importance of Food Taste and Appearance without Forgetting the Safety Factor - Textured Food
8.7.7. Meal Environment and Duration
8.7.8. Adequate Nutritional Value
8.7.9. Diet-Related Support Systems and Support Products
8.7.10. Case Analysis and Decision-Making
8.8. Adaptations and Assistance from Occupational Therapists
8.8.1. Functional Positioning Importance of the "Eater" and "Feeder"
8.8.2. Technical Positioning Aids for Feeders
8.8.3. Technical Positioning Aids for CP People during Feeding
8.8.4. Support Products related to Feeding
8.8.5. Creating Adaptations
8.8.6. Importance of Posture in People on Enteral Nutrition: Relevant Aspects
8.8.7. Participatory Feeding and Autonomy during Feeding
8.8.8. Occupational Therapy and Speech Therapy
8.9. Oropharyngeal Dysphagia in CPC
8.9.1. Referrals and Multidisciplinary Team
8.9.2. Adapting Feeding
8.9.3. Family and Medical Intervention
8.9.4. Assessing Swallowing Process
8.9.5. Individualized Intervention
8.9.6. Texture and Volume Modification as Fundamental Aspects
8.9.7. Sensory Enhancement Techniques
8.9.8. How to Deal with Oral Sensitivity Problems
8.9.9. Postural Changes and Swallowing Facilitating Maneuvers
8.9.10. Drug Intake Aids/Oral Hygiene Products
8.9.11. Importance of Maintaining Intraoral Stimulation in People on Enteral Nutrition
8.10. Nutrition and Cerebral Palsy
8.10.1. Concept of Nutrition: Growth and Development
8.10.2. Relation between Nutrition and Brain Damage, Main Associated Problems
8.10.3. Importance of Maintaining an Adequate Nutritional Intake
8.10.4. Malnutrition, Undernutrition and Dehydration Concepts and Consequences
8.10.5. Basic and Necessary Nutrients
8.10.6. Importance of Nutritional Monitoring and Assessment in CP People
8.10.7. Techniques to Achieve Adequate Nutritional Support; Increased Caloric Density, Oral Modules, Oral Supplementation and Enteral Nutrition
8.10.8. Importance of Person-Centered Nutrition: Individualized Plans
8.10.9. Enteral Nutrition
Module 9. Feeding Problems in Pervasive Developmental Disorders: Autism
9.1. Definition and History
9.1.1. Introduction
9.1.2. Conceptual Review
9.1.2.1. History
9.1.2.2. Prevalence
9.1.2.3. DSM Inclusion
9.1.3. Current Classification
9.1.3.1. Change from DSM-IV to DSM-V
9.1.3.2. Autism Spectrum Disorder 299.00 (F84.0)
9.1.3.3. Conclusions
9.1.3.4. Bibliography
9.2. Early Detection and Diagnosis
9.2.1. Introduction
9.2.2. Social Communication and Interaction
9.2.3. Communication Skills
9.2.4. Social Interaction Skills
9.2.5. Behavioral and Thought Flexibility
9.2.6. Sensory processing
9.2.7. Scales and Instruments
9.2.8. Conclusions
9.2.9. Bibliography
9.3. Heterogeneity in Autism
9.3.1. Introduction
9.3.2. Age-Related Factors
9.3.3. Onset of Signs
9.3.4. Autism in Preschool
9.3.5. Autism in School
9.3.6. Autism in Adolescence
9.3.7. Autism in Adulthood
9.3.8. Sex-Related Factors
9.3.9. Etiology-Related Factors
9.3.10. Conclusions
9.4. Comorbidity
9.4.1. Introduction
9.4.2. Expressive Language Disorders
9.4.3. Most Prevalent Comorbid Disorders
9.4.4. ADHD.
9.4.5. Anxiety and Depression
9.4.6. Obsessions and Compulsions
9.4.7. Dyssomnias and Parasomnias
9.4.8. Movement Abnormalities
9.4.9. Tourette Syndrome
9.4.10. Disorders Associated with ASD in Childhood
9.4.11. High-Functioning Autism
9.4.12. Family and Environment
9.4.13. Conclusions
9.5. Family and Environment Intervention
9.5.1. Introduction
9.5.2. Intervention with Families
9.5.3. Referents to Adapt Family Situation
9.5.4. Environmental Intervention
9.5.5. Family Therapy
9.5.6. Conclusions
9.6. Nutrition in Children with Autism
9.6.1. Introduction
9.6.2. Specific Diet Characteristics
9.6.3. Metabolism
9.6.4. Enzyme Deficiency
9.6.5. Food
9.7. Specific Problems and Inappropriate Intervention Patterns
9.7.1. Not Accepting Spoon Feeding
9.7.2. Leaving Food in the Mouth
9.7.3. Chewing
9.7.4. Hyperselectivity
9.7.5. Crying
9.7.6. Inadequate Guidelines
9.7.7. Recommendations
9.7.8. Conclusions
9.8. Dietary Problems in Children with Autism
9.8.1. Introduction
9.8.2. Strategies
9.8.3. Leading National Work Teams
9.8.4. Intervention Guidelines
9.8.5. Recommendations
9.8.6. Order of Food Introduction
9.8.7. Conclusions
9.9. Clinical Cases: Solid Food Refusal
9.9.1. Medical History Qualitative Assessment of Communication and Language
9.9.2. Structural and Functional Orofacial Assessment
9.9.2.1. Intervention Strategies
9.9.3. Intervention Programs
9.9.4. Respiratory Function
9.9.4.1. Awareness and Control of Respiratory Functions
9.9.4.1.1. Nasal Hygiene
9.9.4.1.2. Postural Hygiene
9.9.4.2. Nasal Breathing and Nasal Murmur
9.9.4.3. Enhancing Olfactory Sensory Response
9.9.5. Dietary Function
9.9.6. Oral Sensitivity
9.9.6.1. Oral Hygiene
9.9.6.2. Oral Stimulation
9.9.7. Oral Motor Skills
9.9.7.1. Oral Stereognosia
9.9.7.2. Gag Reflex Inhibition
9.9.7.3. Taste Stimulation
9.9.8. Masticatory Muscle Relaxation
9.9.9. Chewing without Food
9.9.10. Chewing with Food
9.9.11. Conclusions on Speech Therapy Intervention
9.10. Etiopathogenesis.
9.10.1. Introduction
9.10.2. Endocrine System
9.10.3. Genetics and Heritability
9.10.4. Functional Magnetic Resonance Imaging
9.10.5. Oxytocinergic System
9.10.6. Conclusions
9.10.7. Bibliography
9.10.7.1. Conclusions
9.10.7.2. Bibliography
Improve your skills in tropical diseases through convenient textual and interactive formats that will help you learn in a short period of time"
Hybrid Professional Master’s Degree in Speech Neurorehabilitation and Vital Function Analysis. Orofacial and Myofunctional Therapy
At TECH Global University, we are proud to present our Hybrid Professional Master's Degree in Speech Neurorehabilitation and Vital Functions Analysis. This innovative program is designed specifically for physicians interested in specializing in orofacial and myofunctional therapy. If you want to acquire advanced knowledge and practical skills in this specialized area, this Hybrid Professional Master's Degree is the ideal choice. This program is delivered through a combination of online classes and on-site sessions, giving you the flexibility to study from anywhere while benefiting from direct interaction with experts in speech neurorehabilitation and vital functions analysis. Our online classes offer a dynamic and collaborative platform where you can learn at your own pace, while the face-to-face sessions allow you to apply your knowledge in real clinical situations and receive personalized feedback.
Specialize in sensory stimulation techniques
At TECH Global University, we have a highly qualified and experienced teaching team in the field of speech neurorehabilitation and orofacial therapy. Throughout the Hybrid Professional Master's Degree, you will immerse yourself in the most recent advances in the diagnosis and treatment of orofacial and myofunctional disorders. You will learn specialized techniques to assess and treat conditions such as dysphagia, dysarthria, speech disorder and other related disorders. Our approach combines theory with practice, giving you the opportunity to apply your knowledge in supervised clinical settings. You will learn to use state-of-the-art tools and technologies for vital function analysis and assessment of orofacial function. In addition, you will explore the most effective therapy and rehabilitation strategies, including the use of exercise and sensory stimulation techniques. Upon completion of the Hybrid Professional Master's Degree in Speech Neurorehabilitation and Vital Function Analysis, you will be prepared to provide quality care to patients with orofacial and myofunctional disorders. You will obtain the necessary skills to develop personalized treatment plans, improve the quality of life of your patients and contribute to the advancement of speech neurorehabilitation. Don't miss the opportunity to become an expert in orofacial and myofunctional therapy! Enroll in our Hybrid Professional Master's Degree in Speech Neurorehabilitation and Vital Functions Analysis at TECH Global University and take a step forward in your medical career.







