University certificate
The world's largest faculty of medicine”
Why study at TECH?
Get up to date with the latest diagnostic techniques in Digestive Oncology through this Advanced master’s degree, which will provide you with the most recent advances in the approach to this type of pathology"

In recent years, there has been a significant advance in the understanding of the molecular biology of digestive oncological diseases, which has led to a better understanding of the molecular pathways involved in digestive cancer, allowing the development of new targeted therapies. Given this scenario, the specialist must keep up to date in order to deal with this type of pathology with the latest diagnostic techniques and procedures.
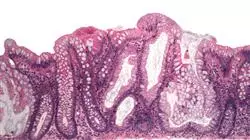
In this context, the Advanced master’s degree in Comprehensive Gastrointestinal Oncology is presented as advanced training for medical professionals who wish to update their knowledge and skills in the field. The program includes fundamental aspects of digestive oncology, from the anatomy and physiology of the gastrointestinal tract to the comprehensive management of digestive cancer patients, including the prevention, diagnosis and treatment of digestive pathologies. In addition, topics such as immunotherapy, molecular biology, new imaging techniques and targeted therapies, which are transforming the treatment of digestive cancers, will be addressed.
The methodology of the program is based on a 100% online format, which allows students to access the contents and resources from anywhere in the world, without the need to travel or fixed schedules. The program has a highly prestigious teaching team, with clinical and teaching experience in digestive oncology, which offers practical and up-to-date training, combining theory with practice and offering innovative tools to improve the clinical performance of the medical professional.
Take advantage of the 100% online methodology with which this programme is developed and access its resources from anywhere and at any time, adapting the study to your needs and schedules"
This Advanced master’s degree in Comprehensive Gastrointestinal Oncology contains the most complete and up-to-date scientific program on the market. The most important features include:
- The development of case studies presented by experts in medicine and oncology
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- Practical exercises where self-assessment can be used to improve learning
- Its special emphasis on innovative methodologies in the approach to digestive oncology
- Theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
Master the latest technologies and surgical techniques in Digestive Oncology and apply them in your daily work thanks to this Advanced master’s degree"
Its teaching staff includes professionals from the field of oncology who bring their experience to this programme, as well as recognised specialists from leading societies and prestigious universities.
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive learning experience designed to prepare for real-life situations.
This program is designed around Problem-Based Learning, whereby the student must try to solve the different professional practice situations that arise throughout the program. For this purpose, the professional will be assisted by an innovative system of interactive videos made by renowned experts.
This program has numerous multimedia resources, such as detailed videos, interactive summaries, interactive in detail, interactive summaries and clinical case studies"
This TECH qualification is taught by highly prestigious specialists in the field of Digestive Oncology"
Syllabus
The syllabus of the Advanced master’s degree in Comprehensive Gastrointestinal Oncology covers the most relevant and up-to-date aspects in the diagnosis and treatment of digestive oncologic diseases. Thus, the specialist will be updated in digestive pathology, from diagnostic and therapeutic endoscopy to advanced surgery. In addition, the latest advances in the diagnosis, treatment and follow-up of neoplasms of the esophagus, stomach, small intestine, colon and rectum, liver and pancreas will be discussed. All this, taught by renowned medical professionals, who will contribute their experience and practical knowledge in each of the subjects.

You are in front of the most complete and updated program in the educational market on Digestive Oncology. Register now and get up to date with the most expert faculty"
Module 1. Molecular Biology and Translational Oncology
1.1. Molecular Mechanisms of Cancer
1.2. Tumor Immunology: Basis of Cancer Immunotherapy
1.3. Role of the Biobank in Clinical Research
1.4. Understanding the New Technology: Next Generation Sequence (NGS) in Clinical Practice
1.5. Liquid Biopsies: Fashion or Future?
1.6. Update on Molecular Markers for Treatment Decisions in Gastrointestinal Malignancies
1.7. Do Molecular and Immunological Classifications Have Clinical Implications Today?
Module 2. Upper Gastrointestinal Tract Tumors
2.1. Differences between Squamous Carcinoma and Esophagus Adenocarcinoma
2.2. Endoscopic Aspects of Esophageal Cancer: Diagnosis and Staging
2.3. Clinical Impact of 18F-FDG PET/CT in the Therapeutic Management of Patients with Esophageal Cancer
2.4. Endoscopic Treatment of Superficial Esophageal Neoplasms
2.5. Conventional Surgical Approach to Esophageal Carcinoma
2.6. Minimally Invasive and Robotic Surgery of Esophageal Cancer
2.7. Evolution in Neoadjuvant and Adjuvant Treatment of Esophageal Cancer
2.8. Management of Metastatic Esophageal Cancer
2.9. Diagnosis and Staging of Gastric Adenocarcinoma
2.10. Minimally Invasive and Robotic Surgery of Gastric Cancer
2.11. Lymphadenectomy Extension in Gastric Cancer
2.12. Neoadjuvant and Adjuvant Treatment in Gastric Cancer: What Is the Optimal Approach?
2.13. The role of radiotherapy treatment in the management of gastric cancer
2.14. National Registry of Advanced Gastric Cancer (AGAMENON)
2.15. First-Line Treatment of HER2-Negative Metastatic Gastric Cancer
2.16. Second-Line Treatment of HER2-Negative Metastatic Gastric Cancer
2.17. Metastatic Gastric Cancer: Impact of Drugs Targeting the HER2 Pathway
2.18. Metastatic Gastric Cancer: Impact of Immune Checkpoint Inhibitors
Module 3. Lower Gastrointestinal Tract Tumors
3.1. Colorectal Cancer: Epidemiology, Etiology and Incidence
3.2. Molecular Mechanisms Involved in the Invasion and Metastasis Process in Digestive Tumors
3.3. Early Detection Program for Colon and Rectum Cancer
3.4. Molecular Classification of Colon Cancer: New insights
3.5. Biomarkers in Colorectal Cancer
3.6. Familial forms of colorectal cancer (polyposis-associated and nonpolyposis-associated)
3.7. Cancer associated with chronic Inflammatory Bowel Diseases and the treatments received
3.8. Diagnosis and Endoscopic Management of Polyps and Advanced Lesions
3.9. Clinical Impact of FDG-PET/CT in the Staging of Colorectal Cancer
3.10. Role of Endoscopic Utrasonography (EUS) and Magnetic Resonance Imaging in the staging of rectal cancer
3.11. Laparoscopic vs. robotic colon cancer surgery
3.12. Surgical Management of Familial Non-Polyposis Colon Cancer
3.13. Surgery for Familial Adenomatous Polyposis
3.14. Current Adjuvant Treatment of Colon Cancer and Proposals for the Future in the Adjuvant Treatment of Colon Cancer
3.15. Total Mesorectal Excision: Open, Laparoscopic and Robotic
3.16. Transanal Approach to Rectal Tumors
3.17. Neoadjuvant Treatment in Rectal Cancer
3.18. Observe and Wait for Low Rectal Cancers after Neoadjuvant Therapy with Complete Clinical Response
3.19. Invasive pelvic tumors: pelvic exenteration
3.20. Therapeutic Advances in Colon and Rectal Cancer: Improving Patient Survival Day by Day
3.21. What Is the Best Treatment Option After Second Line Therapy in Advanced Colorectal Cancer?
3.22. Acquired Resistance to EGFR Antibodies: How to Manage
3.23. Immunotherapy in Metastatic Colorectal Cancer
3.24. Rectal Cancer with Synchronous and Resectable Liver Metastases
3.25. Management of Colorectal Cancer Liver Metastases
3.26. Total excision of the mesocolon: when, how, why
3.27. Role of Endoscopy in the Management of Advanced Colorectal Cancer
Module 4. Other Digestive Tract Tumors
4.1. Appendicular Tumors
4.2. Peritoneal Carcinomatosis
4.3. Treatment of Localized Anal Cancer
4.4. Treatment of Locally Advanced Cancer
4.5. Treatment of Radiation Therapy in Colon Cancer
4.6. Treatment of Metastatic Anal Cancer
4.7. Neuroendocrine Tumors of the Small Intestine
4.8. Neuroendocrine Tumors of the Pancreas
4.9. Surgical Treatment of Non-Functioning Neuroendocrine Pancreas Tumors
4.10. Surgical Treatment of Gastrinoma
4.11. Surgical Treatment of Insulinoma
4.12. Pancreas Endocrine Tumors Surgery: Glucagonoma, Vipoma
4.13. Overview of Systemic Treatment of Metastatic Neuroendocrine Tumors in the Pancreatic Gastroenteropancreatic Tract
4.14. Biology, Diagnosis and Management of Gastrointestinal Stromal Tumors (GIST)
4.15. Surgical Treatment of Gastrointestinal Stromal Tumors (GIST)
4.16. GIST as a Model of Translational Research: 15 Years of Experience
4.17. Gastric MALT Lymphoma
4.18. Lymphomas in Other Digestive Regions
4.19. The Role of 18F-FDG PET/CT in GI Stromal Tumors
Module 5. Pancreatic Cancer, Biliary Tract Tumors and Hepatocarcinoma
5.1. Epidemiology, Risk Factors and Diagnosis of Pancreatic Cancer
5.2. Use of Endoscopic retrograde Cholangiopancreatography (ERCP) in Patients with Pancreatic Masses and Biliary Tract Obstruction
5.3. Use of Endoscopic Ultrasonography (EUS) in Pancreatic Cancer Patients or Pancreatic Masses
5.4. Endosonographic Cholangiopancreatography (CEPEUS) in Pancreatic Masses and Biliary Tract Obstruction
5.5. Diagnostic Modalities for Defining Pancreatic Cancer Resectability (CT, EUS, MRI)
5.6. Clinical Impact of PET/CT with 18F-FDG in the Therapeutic Management of Patients with Pancreas Cancer
5.7. Borderline Resectable Pancreatic Cancer
5.8. Laparoscopic Distal Pancreatectomy: Indications and Technique
5.9. Cephalic pylorus-sparing duodenopancreatectomy versus Whipple in pancreatic cancer
5.10. Surgical Treatment of Ampulomas
5.11. Adjuvant and Neoadjuvant Radiotherapy Treatment for Pancreatic Cancer
5.12. Adjuvant and Neoadjuvant Radiotherapy Treatment for Pancreatic Cancer
5.13. Advances in the Treatment of Patients with Metastatic Pancreatic Cancer
5.14. Screening for Familial and Hereditary Pancreatic Cancer
5.15. Cystic Lesions of the Pancreas of Neoplastic Origin
5.16. Surgery for Cystic Tumors of the Pancreas
5.17. Epidemiology, Risk Factors and Diagnosis of Cholangiocarcinoma and Gallbladder Cancer
5.18. What to Do with Cholangiocarcinoma
5.19. Advances in the Treatment of Patients with Cholangiocarcinoma and Gallbladder Cancer
5.20. Epidemiology, Risk Factors and Diagnoses for Hepatocellular Carcinoma
5.21. Staging and Treatment of Hepatocellular Carcinoma
5.22. Resective Treatment vs. Liver Transplantation in Hepatocellular Carcinoma
5.23. Drainage of Malignant Biliary Obstruction by Interventional Radiology
5.24. First and Second Line of Systemic Therapy in Hepatocellular Carcinoma
5.25. Recurrence of Hepatocellular Carcinoma after Transplantation
5.26. Locally advanced disease with vascular involvement: local versus systemic therapy?
Module 6. Collaboration in the Management of Oncology Patients
6.1. Pre-oncologic assessment in the elderly
6.2. Prescription of Physical Exercise in the Oncologic Patient. Prehabilitation
6.3. Informed Consent: Are We Really Informing Our Patients?
6.4. Palliative Management of Symptoms in Gastrointestinal Tumors
6.5. Palliative Surgical Treatment
6.6. Why do Patients with Gastrointestinal Tumors Attend the Emergency Department and How Can Outcomes Be Improved?
6.7. Management of Infectious Comorbidities
6.8. Management of Cardiovascular Comorbidities
6.9. Neurologic Comorbidity Management
6.10. Management of Endocrinological Comorbidities
6.11. Management of Nutritional Comorbidities
6.12. Gastrointestinal Tumors in the Elderly
6.13. Outpatient Care of Patients with Digestive System Oncology Pathology
Module 7. Oncologic endoscopy
7.1. Chromoendoscopy
7.1.1. Magnification in endoscopy
7.1.2. Classification of injuries in the gastrointestinal tract
7.1.3. Quality Criteria in Endoscopy
7.1.4. Sedation in endoscopy
7.1.5. Management of antiplatelet and anticoagulant medications
7.1.6. Electrosurgical units
7.1.7. Types of prostheses used in oncologic endoscopy
7.2. Online chromoendoscopy
7.2.1. Virtual Chromoendoscopy
7.2.2. Types of Virtual Chromoendoscopy
Module 8. Echoendoscopy and ERCP
8.1. Types of echoendoscopy probes: radial, linear and mini-probe systems
8.2. Types of needle used in echoendoscopy-guided FNA
8.3. Contrast in echoendoscopy
8.4. Gastroenteroanastomosis in the EUS-guided oncologic patient
8.5. Neurolysis of the celiac plexus, alcoholysis and EUS-guided marker placement
8.6. Equipment used during ERCP: cannulas, sphincterotome and balloons
8.7. ERCP techniques: pre-cutting, rendez vous, cytology, biopsy and others
8.8. Ampullary Lesions. Ampulectomy
8.9. Echoendoscopy and ERCP in patients with post-surgical anatomical alterations. Indications and Contraindications
8.10. Complications and their management in EUS and ERCP
Module 9. Resection techniques
9.1. Polypectomy and mucosectomy
9.2. Material used for polypectomy and mucosectomy
9.2.1. Tweezers
9.2.2. Cold and diathermy handles
9.2.3. Programming of electrosurgical unit
9.3. Excision of lesions according to size
9.3.1. Lesions smaller than 20 mm
9.3.2. Lesions larger than 20 mm
9.4. Types of endoscopic mucosal resection
9.5. Endoscopic submucosal Dissection. General Indications
9.6. A Learning Curve
9.7. Material used in endoscopic submucosal dissection
9.7.1. Types of scalpels
9.7.2. Solutions for submucosal injection
9.7.3. Types of caps
9.8. Traction methods
9.9. Subsequent management after excision
9.9.1. Fixation of the lesion
9.9.2. Criteria for curative resection
9.10. Management of complications in lesion resection
9.10.1. Bleeding
9.10.2. Perforation
9.10.3. Cicatricial stenosis
Module 10. Oesophageal
10.1. Risk factors for the development of squamous cell carcinoma and adenocarcinoma
10.2. Barrett's Oesophagus
10.2.1. Diagnosis
10.2.2. Monitoring
10.3. Treatment of Barrett's esophagus
10.3.1. Indications
10.3.2. Resection of visible lesions
10.3.3. Radiofrequency
10.4. Endoscopic features of superficial tumor lesions
10.5. Treatment of superficial esophageal tumor lesions
10.6. Staging of esophageal carcinoma, role of endoscopic ultrasound
10.7. Endoscopic treatment of advanced esophageal carcinoma
10.7.1. Esophageal prosthesis
10.7.2. Gastronomy
10.8. Management of post-surgical complications
10.8.1. Anastomotic stenosis
10.8.2. Suture dehiscence
10.9. Submucosal lesions, diagnosis and treatment
Module 11. Stomach
11.1. Risk factors for the development of gastric cancer and population screening, atrophic gastritis with metaplasia
11.2. Gastric polyps
11.2.1. Fundic gland polyps
11.2.2. Hyperplastic polyps
11.2.3. Adenomatous polyps
11.2.4. Others
11.3. Treatment of Superficial Gastric Neoplasms
11.4. Characteristics of Early Gastric Cancer
11.5. Staging Information About Gastric, Role Gastroesophageal Echoendoscopy Cancer
11.6. Endoscopic management of postoperative complications
11.7. Gastric Lesions GIST, leiomioma
11.8. Treatment of gastric submucosal lesions
11.9. Gastric carcinoids
11.10. Endoscopic findings in hereditary syndromes
11.11. Gastric lymphomas
Module 12. Small Intestine
12.1. Types of small bowel lesions
12.2. Endoscopic capsule
12.3. Capsule endoscopy contraindications and role of Agile Patency
12.4. Single-balloon and double-balloon enteroscopy
12.5. Spiral enteroscopy
12.6. Alternative diagnostic and therapeutic methods to diagnosis with endoscopic techniques
12.7. Endoscopic treatment of superficial tumor lesions
12.8. Management of duodenal polyps and periampullary lesions
12.9. Indications for small bowel exploration in patients with hereditary syndromes
12.10. Intestinal lymphomas
Module 13. Colon and Rectum
13.1. Risk Factors for the Development of Colorectal Cancer
13.2. Population Screening
13.3. Adenomatous polyps of the colon
13.4. Serrated polyps
13.5. Endoscopic characterization of superficial colon neoplasms, risk of submucosal invasion
13.6. Treatment of superficial neoplasms
13.7. Endoscopic follow-up after removal of superficial neoplasms
13.8. Role of endoscopy in the finding of infiltrating neoplasms of the colon
13.8.1. Marking of lesions
13.8.2. Use of prosthesis
13.9. Endoscopic management of complications in rectal surgeries
13.9.1. Stenosis
13.9.2. Suture dehiscence
13.10. Colon cancer screening in inflammatory bowel disease
13.11. Submucosal lesions of colon and rectum
13.12. Endoscopic findings in patients with hereditary syndromes
Module 14. Pancreas
14.1. Adenocarcinoma of the pancreas
14.1.1. Epidemiology, clinical presentation and risk factors
14.1.2. Diagnosis and staging of the disease: role of echoendoscopy
14.2. Endoscopic management (ERCP/USE) of bile duct obstruction in pancreatic cancer
14.3. Endoscopic management of duodenal stricture in pancreatic cancer (prosthesis and gastrojejunal bypass)
14.4. Echoendoscopy-guided treatment options in pancreatic cancer
14.5. Pancreatic cancer screening by echoendoscopy
14.6. Pancreatic neuroendocrine tumors (pNET)
14.6.1. Epidemiological data, classification and risk factors
14.6.2. Role of echoendoscopy in diagnosis, staging, and management
14.6.3. Endoscopic treatment
14.7. Other pancreatic tumors: inflammatory mass, pseudopapillary neoplasm, lymphoma
14.8. Pancreatic cystic tumors
14.8.1. Differential Diagnosis
14.8.2. Serous, mucinous cystadenoma and TPMI
14.9. Role of Endoscopy (EUS and ERCP) in the diagnosis and follow-up of pancreatic cystic lesions
14.10. EUS-guided treatment of pancreatic cystic lesions
Module 15. Gallbladder and bile duct
15.1. Cholangiocarcinoma
15.1.2. Epidemiology and risk factors
15.2. Intrahepatic cholangiocarcinoma
15.2.1. Subtypes and diagnosis
15.3. Extrahepatic cholangiocarcinoma
15.3.1. Clinical Introduction and Diagnosis
15.4. Staging of bile duct tumors, Role of echoendoscopy
15.5. Endoscopic drainage of the biliary tract, role of ERCP
15.6. Endoscopic complications in biliary tract drainage
15.7. Alternatives to endoscopic biliary drainage by ERCP
15.8. Cystic lesions of the biliary tract
15.8.1. Types of biliary cysts
15.8.2. Diagnosis and treatment of biliary cystic lesions
15.9. Gallbladder Carcinoma
15.9.1. Risk Factors
15.9.2. Ultrasound endoscopy as a diagnostic tool
Module 16. Latest advances in endoscopy
16.1. Full-Thickness resection
16.2. Radiofrequency of biliary tract tumors
16.3. Cholangioscopy, use in oncological pathology
16.4. Artificial intelligence to enhance lesion diagnosis during endoscopy
16.5. Endoscopic suture systems, not only for bariatric endoscopy
16.6. Panendoscopy, use of colonic capsule when colonoscopy could not be complete
16.7. Rectal radiofrequency in actinic proctitis after radiotherapy
16.8. Excision of lesions using a combination of surgical and endoscopic techniques
Module 17. Digestive oncologic surgery
17.1. Surgical Anatomy of the Abdomen
17.1.1. Anatomy of the abdominal cavity
17.1.2. Esophagogastric anatomy
17.1.3. Hepatobiliary anatomy
17.1.4. Colorectal anatomy
17.2. Prehabilitation. Multimodal rehabilitation
17.2.1. Prehabilitation
17.2.2. Intraoperative measurements
17.2.3. Postoperative measures
17.3. Fundamentals of Nutrition in Oncologic Digestive Oncologic Surgery
17.3.1. Determination of nutritional status
17.3.2. Consequences of malnutrition
17.3.3. Measures to improve preoperative nutritional status
17.4. Anesthesia in Oncologic Digestive Surgery
17.4.1. Preparation for anesthesia
17.4.2. The importance of anesthesia in Oncologic Surgery
17.4.3. Anesthesia in complex surgeries
17.5. Post-Surgical Resuscitation
17.5.1. Patient optimization after surgery
17.5.2. Detection of early complications
17.5.3. Sepsis and systemic inflammatory response
17.6. Palliative Surgery in Digestive Oncology
17.6.1. What is palliation?
17.6.2. When do we talk about palliation?
17.6.3. Palliative surgical techniques
17.7. Fundamentals of Emergency Surgery in Digestive Oncology
17.7.1. Urgent situations in Oncologic Surgery
17.7.2. Urgent esophagogastric surgery
17.7.3. Urgent hepatobiliary surgery
17.7.4. Urgent colorectal surgery
17.8. Molecular Basis of Digestive Oncology
17.9. Interaction between systemic treatments and surgery
17.9.1. Mechanism of action of systemic oncological treatments
17.9.2. Interaction and consequences on surgery
17.9.3. Measures to minimize surgical complications related to systemic contraction
17.10. Radiation Oncology in Digestive Oncologic Surgery
17.10.1. Fundamental concepts of Radiotherapy
17.10.2. Principles of radiotherapy in the different organs of the digestive tract
17.10.3. Side effects of radiotherapy on the gastrointestinal tract. Prevention and Treatment
Module 18. Complementary studies in digestive tumors
18.1. Role of conventional radiological techniques
18.1.1. Initial Diagnosis
18.1.2. Extension study in patients with digestive tumors
18.1.3. Treatment Plan
18.2. Role of conventional radiology in the early diagnosis and follow-up of patients with digestive tumors
18.2.1. Ultrasound
18.2.2. CAT
18.2.3. MRI
18.3. Role of interventional radiology in digestive tumors
18.3.1. Diagnostic Techniques
18.3.2. Participation in treatment
18.3.3. Role in the management of complications
18.4. Nuclear medicine in the management of digestive tumors
18.4.1. Diagnostic Techniques
18.4.2. Role in treatment
18.4.3. Radioguided Surgery
18.5. Anatomopathologic Diagnosis. Beyond morphology
18.5.1. Importance of intraoperative biopsy
18.5.2. Handling of fresh workpiece and study of margins
18.5.3. Histological risk factors
18.5.4. Standardization of reports
18.6. Molecular Diagnoses
18.6.1. Concept of molecular diagnostics
18.6.2. Cancer panels
18.6.3. From diagnosis to the design of personalized therapies
18.7. Genetic study in patients with risk factors for digestive tumors
18.7.1. Hereditary syndromes associated with digestive tumors
18.7.2. Detection of patients at risk
18.7.3. Follow-up and prophylactic treatment in at-risk patients
18.8. Diagnostic techniques in digestive tumors performed by surgeons
18.9. Microbiome and digestive tumors
18.9.1. Microbiota concept
18.9.2. Role of the microbiome in carcinogenesis
18.9.3. The role of the microbiome in the early diagnosis and prevention of digestive tumors
18.10. Preoperative assessment of the elderly patient
18.10.1. Surgical risk scales
18.10.2. Concept of Fragility
18.10.3. Prehabilitation in the elderly
Module 19. Colorectal oncologic surgery
19.1. Colorectal Cancer
19.1.1. Epidemiology and Etiopathogenesis
19.1.2. Diagnosis and Staging
19.1.3. Follow-up and prognosis of colorectal adenocarcinoma
19.2. Polyposis syndromes
19.2.1. Diagnosis
19.2.2. Treatment
19.2.3. Monitoring
19.3. Endoscopic management of precursor lesions and early cancer
19.3.1. Biliopancreatic Precursor Lesions
19.3.2. Early cancer
19.3.3. Decisions after endoscopic resection
19.4. Surgical treatment of colon cancer. Fundamental concepts about ostomies
19.4.1. Right colon
19.4.2. Transverse colon
19.4.3. Left colon
19.4.4. Colostomies and ileostomies
19.5. Surgical anatomy of the pelvis
19.5.1. General Concepts
19.5.2. Male Pelvis
19.5.3. Female pelvis
19.6. Surgical treatment of rectal cancer
19.6.1. Early Stages
19.6.2. Advanced Stages
19.6.3. Functional sequelae
19.7. Medical Oncology in Colorectal Cancer
19.7.1. Non-metastatic colorectal cancer
19.7.2. Metastatic colorectal cancer
19.7.3. Palliative treatment
19.8. Radiation Oncology in Colorectal Cancer
19.8.1. Radiotherapy in rectal cancer
19.8.2. Radiotherapy in pelvic recurrence
19.8.3. Radiotherapy in special situations
19.9. Total neoadjuvant treatment in rectal cancer. Watch and wait
19.9.1. TNT concept and rationale
19.9.2. Current TNT schemes
19.9.3. Watch and wait concept, handling and indications
19.10. Surgical treatment in special situations
19.10.1. Pelvic relapse of rectal cancer
19.10.2. Positive pelvic adenopathies in rectal cancer
19.10.3. Retroperitoneal lymph node recurrence: Surgery vs. Radiotherapy
Module 20. Esophagogastric oncologic surgery
20.1. General aspects of esophageal cancer
20.1.1. Epidemiology and Etiopathogenesis
20.1.2. classification and diagnosis
20.1.3. Follow-up and prognosis
20.2. Surgical treatment of esophageal cancer
20.2.1. Types of Anastomosis
20.2.2. Standard and extended lymphadenectomy
20.2.3. Alternatives to gastric plasty reconstruction
20.3. Endoscopic and interventional treatment of esophageal cancer
20.3.1. Treatment of precursor lesions
20.3.2. Early cancer treatment
20.3.3. Palliative treatment
20.3.4. Management of complications
20.4. Esophagogastric junction cancer
20.4.1. Controversies in the management of GEU cancer
20.4.2. Approach according to the new clinical guidelines
20.4.3. Lymphadenectomy and surgical approach
20.5. Gastric Cancer Overview
20.5.1. Epidemiology and Etiopathogenesis
20.5.2. classification and diagnosis
20.5.3. Follow-up and prognosis
20.6. Surgical treatment of gastric cancer
20.6.1. Anastomosis
20.6.2. Technical basis of Lymphadenectomy
20.6.3. Treatment of non-adenocarcinoma tumors
20.6.4. Endoscopic treatment
20.7. Oncologic therapies in esophagogastric tumors
20.7.1. Neoadjuvant and adjuvant chemotherapy
20.7.2. Neoadjuvant and adjuvant radiation therapy
20.7.3. New oncology therapies: immunotherapy
20.8. Complications of esophagogastric cancer surgery
20.8.1. Immediate Postoperative Complications
20.8.2. Post-astrectomy sequelae
20.8.3. Poseophagectomy sequelae
20.9. Intensified recovery in esophagogastric surgery
20.9.1. Prehabilitation
20.9.2. Optimization
20.9.3. Clinical pathway
20.10. Research and innovation in esophagogastric oncologic oncologic surgery
Module 21. Innovation, research and development in digestive oncologic surgery
21.1. Basic research in oncological surgery
21.1.1. Introduction to genomics
21.1.2. Introduction to proteomics
21.1.3. Introduction to cytometry
21.2. Platforms for testing new therapies
21.2.1. Animal Models
21.2.2. 2D cellular models
21.2.3. 3D organoid models
21.3. Clinical research in oncological surgery
21.3.1. Clinical trial design
21.3.2. Sources of Financing
21.3.3. Introduction to grant application methodology
21.4. Big data, artificial intelligence and the use of neural networks in oncology research
21.4.1. Introduction to Big Data
21.4.2. Artificial intelligence in oncological surgery
21.4.3. Use of neural networks in oncology research
21.5. Fluorescence techniques and applications in advanced oncologic surgery
21.5.1. Use of fluorescence in oncologic surgery
21.5.2. Techniques of use, doses, times
21.5.3. Results
21.6. Navigation systems, 3D models and intraoperative online virtual reality in the oncologic disease approach
21.6.1. Browsing Systems
21.6.2. Utility and application of 3D models
21.6.3. Intraoperative online virtual reality
21.7. Minimally invasive approach in complex oncologic surgery
21.7.1. Minimally invasive approach concept and modalities
21.7.2. Description of the different modalities
21.7.3. Robotics
21.8. Intraoperative ablative and adjuvant techniques in oncologic surgery
21.8.1. Intraoperative ablation techniques: mechanism of action
21.8.2. Differences, advantages and disadvantages
21.8.3. Intraoperative radiotherapy
21.9. Liquid biopsy and circulating DNA as diagnostic and prognostic methods in advanced neoplastic disease
21.9.1. What is liquid biopsy?
21.9.2. How is a liquid biopsy performed?
21.9.3. Liquid biopsy applications
21.10. New oncology treatment lines
21.10.1. Target therapy in digestive oncology and sarcomas
21.10.2. Immunotherapy in digestive tumors
21.10.3. CAR-T Therapy

The teaching materials of this program, elaborated by these specialists, have contents that are completely applicable to your professional experiences”
Advanced Master's Degree in Comprehensive Gastrointestinal Oncology
Gastrointestinal cancer is a complex disease that requires specialization and a comprehensive approach for its diagnosis and treatment. At TECH Global University, we have developed the Advanced Master's Degree in Comprehensive Gastrointestinal Oncology, an online program designed to provide health professionals with the necessary tools to face the challenges of this pathology in clinical practice. This program focuses on updating the latest knowledge in early diagnosis, multimodal treatment and follow-up of patients with gastrointestinal cancer. In addition, the management of minimally invasive surgical techniques, targeted therapies and management of side effects of chemotherapy and radiotherapy in the context of gastrointestinal oncology will be discussed in depth.
The postgraduate program comprehensively addresses the different areas of gastrointestinal oncology, including cancer of the esophagus, stomach, small intestine, colon, rectum, liver and pancreas. Program participants will have the opportunity to interact with experts in the field, share experiences and learn from real clinical cases. This program is designed for medical oncologists, digestive surgeons, gastroenterologists and other health professionals interested in updating and improving their knowledge in the comprehensive approach to digestive cancer. Take advantage and improve your résumé with TECH.







