University certificate
The world's largest faculty of medicine”
Why study at TECH?
Discover the latest updates in gynecologic cancer biology and treatment with this Advanced master’s degree in Integrative Gynecologic Oncology”

Today, gynecologic cancer represents a significant challenge to women's health worldwide. With the constant evolution in the understanding of the biology and pathology of these tumors, as well as diagnostic and treatment strategies, it is essential for medical specialists to be up-to-date on the latest advances in gynecologic oncology. The complexity and multidisciplinary nature of the care of these patients requires a comprehensive approach that addresses not only clinical aspects, but also psychosocial, ethical and quality of life aspects.
Against this backdrop, TECH has created this Advanced master’s degree in Integrative Gynecologic Oncology. This is an update option for all specialists interested in deepening their knowledge in this field. The program syllabus includes a solid knowledge base in the biological basis of cancer, as well as in chemotherapy treatment, adverse effects and new therapies. The specific management of different types of gynecological cancers, such as endometrial, cervical, ovarian and vulvar cancer, as well as uterine sarcomas, is discussed in depth.
The program has a team of highly trained teachers with extensive experience in the management of gynecological cancer, which guarantees quality and updated teaching. Furthermore, an educational methodology based on active and participatory teaching is used, with the use of clinical cases, group discussions and practical activities that allow participants to apply the knowledge acquired in real clinical situations.
A significant advantage of the program is its comprehensive approach, which encompasses clinical, surgical, radiotherapeutic, oncologic and quality-of-life aspects of gynecologic cancer management. Participants will gain a holistic view of the disease and its approach, in a 100% online format that gives them the flexibility to combine it with their personal and professional lives.
You will have a highly qualified teaching team with extensive experience in the management of gynecological cancer, guaranteeing quality and updated teaching”
This Advanced master’s degree in Integrative Gynecologic Oncology contains the most complete and up-to-date scientific program on the market. The most important features include:
- Practical case studies are presented by experts in and Oncology and Gynecology
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- Practical exercises where self-assessment can be used to improve learning
- A special emphasis on innovative methodologies in the Gynecological Oncology
- Theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
You will cover not only the clinical, but also the psychosocial, ethical and quality of life aspects of gynecologic cancer management, providing you with a holistic view of the disease”
Its teaching staff includes professionals from the field of education, who bring to this program the experience of their work, as well as recognized specialists from reference societies and prestigious universities.
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive learning experience designed to prepare for real-life situations.
This program is designed around Problem-Based Learning, whereby the student must try to solve the different professional practice situations that arise throughout the program. For this purpose, the professional will be assisted by an innovative interactive video system created by renowned and experienced experts.
You will have clinical cases and practical activities that will allow you to apply the knowledge acquired in real clinical situations”
With a 100% online format, you can study at your own pace and combine it with your personal and professional life, without compromising your daily responsibilities”
Syllabus
The program includes high quality multimedia material, such as work guides, detailed videos and interactive resources, which enrich the participant's learning experience and facilitate the understanding of key concepts. Specialists will have access to a wide variety of educational resources that complement the theoretical classes, which will allow them to deepen their knowledge of the topics in a practical and applied manner.

Access workbooks, detailed videos and other high-quality interactive resources to enrich your learning experience”
Module 1. Biological Basis of Cancer
1.1. Cell Growth Regulation
1.2. Carcinogenesis and Carcinogens
1.3. Genetics of Cancer
1.4. Mechanisms of Apoptosis and Programmed Cell Death
1.5. Molecular Mechanisms of Cancer Production and Metastasis
1.6. Origin of Genetic Alterations
1.7. Epigenetic Changes and Oncogenes
1.8. Angiogenesis
Module 2. Basis of Chemotherapy Treatment, Adverse Affects and New Therapies
2.1. Introduction
2.2. Justification for the Use of Chemotherapy
2.3. Development of Cancer and the Influence of Chemotherapy
2.3.1. Tumor Growth
2.3.2. Cellular Cycle
2.3.3. Specific Drugs for each of the Cellular Phases
2.4. Factors that Influence Treatment
2.4.1. Tumor Characteristics
2.4.2. Patient Tolerence
2.4.3. Treatment Objectives
2.4.4. Pharmacological Factors and Administration Routes
2.5. Principles of Resistance to Drugs
2.6. Combined Therapies
2.7. Treatment or Dosis Adjustments
2.8. Drug Toxicity
2.9. General Management of Secondary Effects and Complications of Chemotherapy
2.10. Antineoplastic Agents in Gynecology
2.10.1. Alkylating Agents
2.10.2. Antibiotics
2.10.3. Antimetabolites
2.10.4. Plant Alkaloids
2.10.5. Topoisomerase 1 Inhibitors
2.10.6. Antiangiogenic Drugs
2.10.7. PARP Inhibitors
2.10.8. Tyrosine Kinase Inhibitors
2.10.9. Other Drugs
2.11. Future Indications
Module 3. Endometrial Cancer I
3.1. Epidemiology and Etiopathogenesis
3.2. Precancerous Lesions
3.3. Hereditary Carcinoma
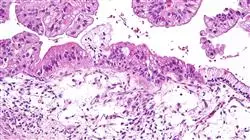
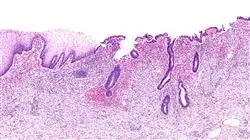
3.4. Pathological Anatomy and Different Types of Tumors
3.5. Diagnostic Process
3.6. Imaging Tests, Tumor Markers and Possible Screening
3.7. Molecular Diagnostic Tests
3.8. FIGO Clasiffication and Others
Module 4. Endometrial Cancer II
4.1. Introduction
4.2. General Aspects of Surgical Treatment
4.3. Low Risk Tumors (Stage I, Grade 1)
4.4. High Risk Tumors (Grade 2-3, Serous or Clear Cells)
4.5. Laparotomy vs. Laparoscopy
4.6. Introduction of Robotic Surgery
4.7. Surgical Technique for High Risk Tumors
4.8. Adjuvant Treatment
4.8.1. Observation without Additional Treatment
4.8.1.1. Low Risk, Early Stage, Low Grade
4.8.2. Adjuvant Radiotherapy
4.8.2.1. Early Stage, Intermediate and High Risk
4.8.2.2. Advanced Stages
4.8.3. Adjuvant Chemotherapy
4.8.4. Peculiarities of Serous Tumors and Clear Cells
4.9. Hormonal Treatment
4.10. Recurrent Endometrial Cancer
4.10.1. Surgical Management
4.10.2. Radiotherapy
4.10.3. Chemotherapy
4.11. Follow-up Treatment of Endometrial Cancer
4.12. Prognosis
Module 5. Cervical Cancer I
5.1. Epidemiology and Etiopathogenesis of the Disease
5.2. Precancerous Lesions and the Evolutionary Process
5.3. Risk Factors for Contracting the Disease
5.4. Notions about Cervical Pathology and HPV
5.5. Normal Colposcopy and Vulvoscopy
5.6. Abnormal Colposcopy and Vulvoscopy
5.7. Cervical Cancer Screening
5.8. Hereditary Carcinoma
5.9. Forms of Presentation in Anatomic Pathology
5.10. Diagnostic Process: Imaging Tests and Tumor Markers
5.11. Role of New Technologies such as PET-CT
5.12. FIGO and TNM Classification in Cervical Carcinoma
Module 6. Cervical Cancer II
6.1. Treatment of Cervical Intraepithelial Neoplasia (CIN)
6.1.1. CIN Surgery
6.1.2. CIN Immunotherapy
6.2. Invasive Treatment of Cervical Cancer
6.2.1. Radical Hysterectomy with Nerve Preservation
6.2.2. Less Radical Hysterectomy
6.2.3. Radical Endoscopic Hysterectomy
6.2.4. Selective Sentinel Node Biopsy
6.2.5. Para-Aortic Advanced Stage Lymphadenectomy Staging
6.3. Radiotherapy and Chemotherapy
6.3.1. Concurrent Chemoradiotherapy
6.3.2. Enhanced Radiation Therapy Treatment Modalities
6.3.3. Chemotherapy Modalities in Concurrent Treatment
6.3.4. Preoperative Chemoradiotherapy
6.3.5. Adjuvant Therapy after a Radical Hysterectomy
6.3.6. Neoadjuvant Chemotherapy
6.3.7. Adjuvant Therapy after Neoadjuvant and Previous Surgery
6.4. Treatment of Metastasis, Recurrent or Persistent Disease
6.4.1. Surgical Management
6.4.2. Chemotherapy
6.5. Management of Cervical Adenocarcinoma
6.5.1. Adenocarcinoma in Situ (AIS)
6.5.2. Comparison Between Squamous Cell Carcinomas and Adenocarcinomas
6.5.3. Surgery vs. Radiotherapy in Invasive Adenocarcinoma
6.5.4. Chemotherapy
6.6. Monitoring
Module 7. Ovarian Cancer I
7.1. Epidemiology of Ovarian and Fallopian Tube Cancer
7.2. Etiopathogenesis and tubal origin, new trends
7.3. Precancerous Lesions in the Fallopian Tubes
7.4. Ovarian Cancer Screening
7.5. Hereditary Carcinoma and How to Evaluate It
7.6. Histological Forms and Pathological Anatomy
7.7. Diagnostic Process
7.7.1. Clinical Symptoms
7.7.2. Ultrasound
7.7.3. Computerized Tomography
7.7.4. Magnetic Resonance
7.7.5. Positron Emission Tomography
7.8. Serum Tumor Markers
7.8.1. CA125
7.8.2. HE4
7.8.3. CA19.9.
7.8.4. CEA
7.8.5. Other Markers
7.9. FIGO Classification of the Disease
Module 8. Ovarian Cancer II
8.1. General Surgical Treatment
8.2. Complete Cytoreduction and Primary Debulking
8.3. Neoadjuvant Treatment and When to Choose It
8.4. Interval and Second Look Treatments
8.5. Adjuvant Therapy: Carboplatin-Taxol and Other Options
8.6. Radiotherapy: What Role Does it Play?
8.7. Hormonal Therapy Possibilities in Ovarian Cancer
8.8. Prognosis and Disease-Free Interval
8.9. Monitoring and Treatment of Relapses
8.10. Controversies in the Management of Ovarian Cancer
8.11. Peritoneal Carcinomas Hyperthermic Therapy
8.12. Intraperitoneal Chemotherapy, Indications and Results
Module 9. Vulvar Cancer I
9.1. Epidemiology and Relationship with HPV
9.2. Etiopathogenesis and Precancerous Lesions
9.3. VIN I, II, III VAIN and Other Lesions
9.4. Vulvar Cancer Screening
9.5. Hereditary Carcinoma
9.6. Anatomical Pathology and Histological Types
9.7. Imaging Tests and Extension Study
9.8. Tumor Markers: SCC
Module 10. Vulvar Cancer II
10.1. Introduction
10.2. Vulvar Paget’s Disease
10.2.1. General Aspects
10.2.2. Paget’s Disease Type 1
10.2.2.1. Prevalence
10.2.2.2. Clinical Characteristics
10.2.2.3. Diagnosis
10.2.2.4. Treatment
10.2.3. Paget’s Disease Type 2 and 3
10.3. Invasive Paget’s Disease
10.3.1. General Aspects
10.3.2. Prognosis
10.4. Invasive Vulva Carcinoma
10.4.1. Squamous Cell Carcinoma
10.4.2. Clinical Characteristics
10.4.3. Diagnosis
10.4.4. Dissemination Pathways
10.4.5. Staging
10.4.6. Treatment
10.4.6.1. Primary Lesion Management
10.4.6.2. Local Control after Primary Surgical Treatment
10.4.6.3. Management of Ganglionic Chains
10.4.6.4. Post-Operative Care
10.4.6.4.1. Early postoperative complications
10.4.6.4.2. Late Postoperative Complications
10.4.6.5. Use of Sentinel Lymph Node
10.4.6.5.1. Advanced Disease
10.4.6.5.2. General Aspects
10.4.6.5.3. Management of Ganglionic Chains
10.4.6.5.4. Management of Primary Tumor
10.4.6.5.4.1. Surgery
10.4.6.5.4.2. Radiotherapy
10.4.6.5.4.3. Chemotherapy
10.4.6.6. Role of radiotherapy in vulvar cancer
10.4.7. Recurrent Vulvar Cancer
10.4.8. Prognosis
10.4.9. Monitoring
10.5. Vulva Melanoma
10.5.1. Introduction
10.5.2. Clinical Characteristics
10.5.3. Pathologic Anatomy
10.5.4. Staging
10.5.5. Treatment
10.5.5.1. Primary Lesion Management
10.5.5.2. Management of Ganglionic Chains
10.5.6. Prognosis
10.6. Bartholin’s Gland Carcinoma
10.6.1. General Aspects
10.6.2. Treatment
10.6.3. Prognosis
10.7. Basal Cell Carcinoma
10.8. Verrucous Carcinoma
10.9. Vulva Sarcoma
10.9.1. Introduction
10.9.2. Leiomyosarcoma
10.9.3. Epithelioid Sarcoma
10.9.4. Rhabdomyosarcoma
10.9.5. Merkel Cells Carcinoma
Module 11. Uterine Sarcoma I
11.1. Introduction
11.2. Epidemiology
11.2.1. Incidence
11.2.2. Age
11.2.3. Histological Distribution
11.2.4. Racial Distribution
11.3. Risk Factors
11.3.1. Heritage
11.3.2. Hormone Therapy
11.3.3. Radiation Exposure
11.4. Pathologic Anatomy
11.4.1. Leiomyosarcoma
11.4.2. STUMP
11.4.3. Benign Metastasizing Leiomyoma
11.4.4. Carcinosarcoma
11.4.5. Endometrial Stromal Neoplasms
11.4.6. Stromal Nodule
11.4.7. Endometrial Stromal Sarcoma
11.4.8. Mullerian Adenosarcoma
11.5. Clinical Manifestations
11.6. Imaging Tests
11.6.1. Magnetic Resonance
11.6.2. Tumor Markers
11.7. FIGO Staging
11.8. Conclusions
Module 12. Uterine Sarcoma II
12.1. Introduction
12.2. Uterine Leiomyosarcoma
12.2.1. Early Stages
12.2.1.1. Surgery
12.2.1.2. Adjuvant Radiotherapy
12.2.1.3. Chemotherapy
12.2.2. Recurrent or Metastatic Disease
12.2.2.1. Surgery
12.2.2.2. Chemotherapy
12.2.2.3. Hormone Therapy
12.2.3. Prognostic Factors
12.3. Endometrial Stromal Sarcoma
12.3.1. Early Stages
12.3.1.1. Surgery
12.3.1.2. Pelvic Radiotherapy
12.3.1.3. Hormone Therapy
12.3.2. Recurrent or Metastatic Disease
12.3.2.1. Surgery
12.3.2.2. Chemotherapy or Radiotherapy
12.3.3. Prognostic Factors
12.4. Undifferentiated Endometrial Sarcoma
12.4.1. Early Stages
12.4.1.1. Surgery
12.4.1.2. Adjuvant Radiotherapy
12.4.1.3. Chemotherapy
12.4.2. Recurrent or Metastatic Disease
12.4.2.1. Surgery
12.4.2.2. Chemotherapy or Radiotherapy
12.4.3. Prognostic Factors
12.5. Conclusions
Module 13. Fertility Preservation
13.1. Indications of Fertility Preservation
13.2. Gametes Preservation
13.3. Role of Assisted Reproduction Techniques
13.4. Conservative Surgical Treatment
13.5. Oncological Prognosis after Fertility Conservation
13.6. Reproductive Results
13.7. Dealing with Pregnant Women with Gynecologic Cancer
13.8. New research paths and literature updates
13.9. Conservation of Ovarian Tissue
13.10. Uterine and Gonadal Tissue Transplantation
Module 14. Uncommon Gynecologic Tumors
14.1. Vagina Cancer
14.1.1. Introduction
14.1.2. Clinical Manifestations
14.1.3. Diagnosis
14.1.4. Pathologic Anatomy
14.1.4.1. Squamous Carcinoma
14.1.4.2. Adenocarcinoma
14.1.4.3. Sarcoma
14.1.4.4. Melanoma
14.1.5. Tumor Staging
14.1.6. Treatment of Disease
14.1.6.1. Surgery
14.1.6.2. Radiotherapy
14.1.6.3. Treatment Complications
14.1.7. Monitoring
14.1.8. Prognosis
14.2. Gestational Trophoblastic Disease
14.2.1. Introduction and Epidemiology
14.2.2. Clinical Forms
14.2.2.1. Hydatidiform Mole
14.2.2.1.1. Complete Hydatidiform Mole
14.2.2.1.2. Partial Hydatidiform Mole
14.2.2.2. Gestational Trophoblastic Neoplasm
14.2.2.2.1. After Molar Pregnancy
14.2.2.2.1.1. Persistent Gestational Trophoblastic Neoplasm
14.2.2.2.2. After Non-Molar Pregnancy
14.2.2.2.2.1. Choriocarcinoma
14.2.2.2.2.2. Placental Site Trophoblastic Tumor
14.2.3. Diagnosis
14.2.3.1. Human Chorionic Gonadotropin
14.2.3.2. Ultrasound Study
14.2.3.2.1. Complete Mole
14.2.3.2.2. Partial Mole
14.2.3.2.3. Invasive Mole
14.2.3.2.4. Choriocarcinoma and Placental Site Tumor
14.2.3.3. Other Imaging Techniques
14.2.4. Pathologic Anatomy
14.2.4.1. Hydatidiform Mole
14.2.4.1.1. Complete Mole
14.2.4.1.2. Partial Mole
14.2.4.2. Invasive Mole
14.2.4.3. Choriocarcinoma
14.2.4.4. Placental Site Trophoblastic Tumor
14.2.4.5. Epithelioid Trophoblastic Tumor
14.2.5. Staging
14.2.6. Treatment
14.2.6.1. Chemotherapy
14.2.6.1.1. Low Risk Disease
14.2.6.1.2. High Risk Disease and Metastasis
14.2.6.1.3. Chemoresistant Disease
14.2.6.2. Surgery
14.2.6.2.1. Molar Evacuation
14.2.6.2.2. Hysterectomy
14.2.6.2.3. Myometrial Resection
14.2.6.2.4. Pulmonary Resection
14.2.6.2.5. Craniotomy
14.2.6.2.6. Other Surgical Procedures
14.2.6.2.7. Selective Arterial Embolization
14.2.7. Post-Treatment Monitoring
14.2.7.1. Monitoring after Molar Evacuation
14.2.7.2. Monitoring after Gestational Neoplasm Treatment
14.2.8. Prognosis
14.3. Metastatic Tumor in the Genital Tract
14.3.1. Introduction
14.3.2. Clinical Manifestations
14.3.2.1. Secondary Tumors in the Uterine Body or Cervix
14.3.2.2.1. From Genital or Pelvic Organs
14.3.2.2.2. From Extragenital or Pelvic Organs
14.3.2.2. Secondary Tumors in the Vagina
14.3.2.3. Secondary Tumors on the Vulva
14.3.2.4. Secondary Tumors in the Ovaries
14.3.3. Diagnosis
14.3.4. Pathologic Anatomy
14.3.4.1. Gastrointestinal Tumors
14.3.4.1.1. Metastasis of Intestinal Cancer
14.3.4.1.2. Krukenberg Tumor
14.3.4.2. Ovarian Lymphona
14.3.5. Treatment and Prognosis
14.4. Neuroendocrine Tumors
14.4.1. Introduction
14.4.2. Pathologic Anatomy
14.4.2.1. Well-Differentiated Tumors
14.4.2.2. Poorly-Differentiated Tumors
14.4.3. Clinical Manifestations and Diagnosis
14.4.3.1. Small Cell Tumor in the Vulva and Vagina
14.4.3.2. Small Cell Tumor in the Uterus
14.4.3.3. Neuroendocrine Tumors in the Cervix
14.4.3.3.1. Small Cell Neuroendocrine Carcinoma
14.4.3.3.2. Carcinoma neuroendocrino células grandes
14.4.3.4. Ovarian, Fallopian Tube and Wide Ligament Tumor
14.4.3.4.1. Ovarian Carcinoid
14.4.3.4.1.1. Insular Carcinoid
14.4.3.4.1.2. Trabecular Carcinoid
14.4.3.4.1.3. Mucinous Carcinoid
14.4.3.4.1.4. Strumal Carcinoid
14.4.3.4.2. Small Cell Lung Type
14.4.3.4.3. Undifferentiated Non-Small Cell Carcinoma
14.4.4. Treatment
14.4.5. Monitoring
14.4.6. Prognosis
14.5. Rectovaginal Septum Tumors
Module 15. Palliative Care and Nutrition
15.1. Introduction
15.1.1. Symptomology Associated with Gynecologic Tumors
15.2. Pain
15.3. Gastrointestinal Symptoms
15.3.1. Diarrhea
15.3.2. Constipation
15.3.3. Malignant Intestinal Obstruction
15.3.3.1. Conservative Treatment
15.3.3.2. Surgical Management
15.4. Ascites
15.5. Respiratory symptoms
15.5.1. Pleural Effusion
15.6. Edema
15.7. Anorexia and Weight Loss
15.8. Deep Vein Thrombosis
15.9. Pelvic Disease Progression
15.9.1. Vaginal Bleeding
15.9.2. Fistulas
15.10. Palliative Pelvic Exenteration
15.11. Metastasis of Other Organs
15.11.1. Liver
15.11.2. Brain
15.11.3. Bone
15.11.3.1. Hypercalcemia
15.12. Anxiety and Depression
15.13. Dying Patient Care
Module 16. Diagnostics in Mastology
16.1. Introduction to Imaging Diagnosis in Mastology
16.2. Radiological Interpretation in Breast Pathologies
16.3. Nodule and Asymmetries Breasts
16.4. Diagnostic Management of Microcalcifications and Distortion of the Breast Architecture
16.5. Mammary Interventionism
16.6. Pre-Treatment Clinical Staging in Breast Cancer
16.7. Other Indications of Mammary Magnetic Resonance
16.8. Treated and Operated Breast
16.9. Rare Breast Pathology. Special Situations
16.10. Advances in Mammary Diagnosis and Interventionism
Module 17. Pathologic Anatomy
17.1. Introduction to Breast Pathological Anatomy
17.1.1. Concepts. Anatomopathological Language
17.1.2. Methods for Studying Pathological Anatomy
17.1.3. Types of Samples
17.1.4. Clinical and Radiological Correlation
17.1.4.1. Surgical Specimen Orientation
17.1.5. Diagnosis: The Anatomopathological Report
17.1.6. Normal Breast
17.2. Benign Epithelial Tumors Papillary Neoplasms Premalignant Lesions
17.2.1. Benign Epithelial Proliferations and Precursors
17.2.1.1. Usual Ductal Hyperplasia
17.2.1.2. Columnar Cell Lesions, Including Flat Epithelial Atypia
17.2.1.3. Atypical Ductal Hyperplasia
17.2.2. Adenosis and Benign Sclerosing Lesions
17.2.2.1. Sclerosing Adenosis
17.2.2.2. Adenosis and Apocrine Adenoma
17.2.2.3. Adenosis Microglandular
17.2.2.4. Radial Scar and Complex Sclerosing Lesion
1 7.2.3. Adenomas
17.2.3.1. Tubular Adenoma
17.2.3.2. Lactational Adenoma
17.2.3.3. Ductal Adenoma
17.2.4. Epithelial-Myoepithelial Tumors
17.2.4.1. Pleomorphic Adenoma
17.2.4.2. Adenomyoepithelioma
17.2.5. Papillary Neoplasms
17.2.5.1. Intraductal Papilloma
17.2.5.2. Papillary Ductal Carcinoma in situ
17.2.5.3. Encapsulated Papillary Carcinoma
17.2.5.4. Solid Papillary Carcinoma in situ
17.2.6. Non-Invasive Lobular Neoplasia
17.2.6.1. Atypical Lobular Hyperplasia
17.2.6.2. Lobular Carcinoma in situ
17.2.7. Ductal Carcinoma in situ
17.3. Malignant Epithelial Tumors
17.3.1. Infiltrating Carcinoma and Subtypes
17.3.1.1. Infiltrating Carcinoma Without a Special Subtype
17.3.1.2. Microinfiltrating Carcinoma
17.3.1.3. Infiltrating Lobular Carcinoma
17.3.1.4. Tubular Carcinoma
17.3.1.5. Cribriform Carcinoma
17.3.1.6. Mucinous Carcinoma
17.3.1.7. Mucinous Cystadenocarcinoma
17.3.1.8. Infiltrating Micropapillary Carcinoma
17.3.1.9. Infiltrating Solid Papillary Carcinoma
17.3.1.10. Infiltrating Papillary Carcinoma
17.3.1.11. Carcinoma with Apocrine Differentiation
17.3.1.12. Metaplastic Carcinoma
17.3.2. Saliva Gland Type Carcinomas
17.3.2.1. Acinar Cell Carcinoma
17.3.2.2. Adenoid Cystic Carcinoma
17.3.2.3. Secretor Carcinoma
17.3.2.4. Mucoepidermoid Carcinoma
17.3.2.5. Polymorphous Adenocarcinoma
17.2.2.6. Tall Cell Carcinoma with Reverse Polarization
17.3.3. Neuroendocrine Neoplasms
17.3.3.1. Neuroendocrine Tumor
17.3.3.2. Neuroendocrine Carcinoma
17.4. Fibroepithelial Tumors Nipple-areola complex Tumors Hematolymphoid Tumors
17.4.1. Fibroepithelial Tumors
17.4.1.1. Hamartoma
17.4.1.2. Fibroadenoma
17.4.1.3. Tumor Phyllodes
17.4.2. Nipple-areola Complex Tumors
17.4.2.1. Syringomatous Tumor
17.4.2.2. Nipple Adenoma
17.4.2.3. Paget’s Disease of the Breast
17.4.3. Hematolymphoid Tumors
17.4.3.1. MALT Lymphoma
17.4.3.2. Follicular Lymphoma
17.4.3.3. Diffuse Large B-cell Lymphoma
17.4.3.4. Burkitt Lymphoma
17.4.3.5. Anaplastic Large Cell Lymphoma Associated with Breast Implantation
17.5. Mesenchymal Tumors
17.5.1. Vascular Tumours
17.5.1.1. Hemangioma
17.5.1.2. Angiomatosis
17.5.1.3. Atypical Vascular Lesions
17.5.1.4. Primary Angiosarcoma
17.5.1.5. Post-Radiation Angiosarcoma
17.5.2. Fibroblastic and Myofibroblastic Tumors
17.5.2.1. Nodular Fascitis
17.5.2.2. Myofibroblastoma
17.5.2.3. Desmoid Fibromatosis
17.5.2.4. Inflammatory Myofibroblastic Tumor
17.5.3. Peripheral Nerve Sheath Tumors
17.5.3.1. Schwannoma
17.5.3.2. Neurofibroma
17.5.3.3. Granular Cells Tumor
17.5.4. Smooth Muscle Tumors
17.5.4.1. Leiomyoma
17.5.4.2. Leiomyosarcoma
17.5.5. Adipocytic Tumors
17.5.5.1. Lipoma
17.5.5.2. Angiolipoma
17.5.5.3. Liposarcomas
17.6. Clinical Pathological Special Situations Genetic Tumor Syndromes
17.6.1. Clinical Pathological Special Situations
17.6.1.1. Young Woman
17.6.1.2. Pregnancy and Lactation
17.6.1.3. Elderly Woman
17.6.1.4. Men
17.6.1.5. Hidden
17.6.1.6. Inflammatory Carcinoma
17.6.2. Genetic Tumor Syndromes
17.6.2.1. BRCA1/2-Associated Hereditary Breast and Ovarian Cancer Syndrome
17.6.2.2. Cowden Syndrome
17.6.2.3. Ataxia-Telangiectasia
17.6.2.4. TP53-Associated Li-Fraumeni Syndrome
17.6.2.5. CHEK2-Associated Li-Fraumeni Syndrome
17.6.2.6. CDH1-Associated Breast Cancer
17.6.2.7. Cancer Associated with PALB2
17.6.2.8. Peutz-Jeghers Syndrome
17.6.2.9. Neurofibromatosis Type I
17.7. Non-Tumorous Pathology
17.7.1. Pseudoangiomatous Stromal Hyperplasia
17.7.2. Diabetic Mastopathy
17.7.3. Fibrosis
17.7.4. Mondor Disease
17.7.5. Changes Due to Breastfeeding
17.7.6. Mastitis
17.7.6.1. Mastitis Granulomatosa
17.7.6.2. Mastitis Non-Granulomatosa
17.8. Prognosis
17.8.1. Tumor Grade
17.8.2. Pathological Staging
17.8.3. Surgical Border
17.8.4. Sentinel Lymph Node
17.8.4.1. OSNA
17.8.5. Treatment-Oriented Immunohistochemistry Classes
17.8.6. Nomograms
17.8.6.1. Cases
17.9. Prediction
17.9.1. Evaluation of Response to Neoadjuvant Treatment
17.9.2. Prediction of the Response to Chemotherapy Treatment
17.9.2.1. Genetic Platforms Oncotye DX, Mamaprint, PAM50
17.9.3. Therapeutic Targets
17.9.4. NGS
17.9.5. Digital and Computational Pathology
17.9.5.1. Cases
17.10. Multimodality
17.10.1. Positive, Negative or Uncertain
17.10.2. Interpretation of Data in the Clinical Context
17.10.2.1. Statistics and Probability
17.10.3. Quality Control
17.10.3.1. Protocols
17.10.4. Pathologists in the Breast Unit
17.10.4.1. Difficult Cases: are tumors, occult primary, non-breast OSNA, very long monitoring processes
17.10.5. Conclusions
Module 18. Functional Anatomy
18.1. Radiological Anatomy of the Mammary Region
18.2. Radiological Anatomy of the Donor Regions in Reconstructive Breast Surgery
18.3. Surgical Anatomy in Oncology and Reconstructive Surgery Topography, Anatomic Relations
18.4. Muscular Surroundings
18.5. Arterial and Venous Vascularization
18.5.1. Key Points of Vascularization in the Conservation of Skin and Areola
18.5.2. Key Points of Vascularization in the Muscular Preservation and Local Flaps
18.6. Lymphatic Drainage
18.7. Innervation
18.8. Axillary Cavity
18.8.1. Limits
18.8.2. Vascular Content
18.8.3. Nerve Content
18.8.4. Ganglionic Content, Berg Levels, Surgical Approaches to the Axilla
18.9. Internal Mammary Role in Free Flaps
18.10. Supraclavicular Region
Module 19. Embriology, Malformations, Intersexual States
19.1. Embryology
19.2. Physiology
19.3. Mammary malformations
19.3.1. Polymastia
19.3.2. Muscle Abnormalities and Agenesis Poland Syndrome
19.3.3. Tubular Breasts
19.3.4. Alterations of the Nipple-areola Complex
19.4. Macromastia and Micromastia
19.5. Gynecomastia
19.6. Intersexual Syndromes
19.7. Breast Cancer in Childhood and Adolescence:
19.7.1. Environmental Causes
19.7.2. Genetic Causes
19.8. Inflammatory Disease
19.8.1. Acute Mastitis Abscess
19.8.2. Chronic Mastitis
19.8.3. Mondor Disease
19.8.4. Plasmatic Cell Mastitis
19.8.5. Periductal Mastitis
19.9. Systemic
19.9.1. Sarcoidosis
19.9.2. Granulomatosis
19.10. Burns in the Mammary Area in Childhood and Adolescence
Module 20. Locoregional Surgical Treatment in Malignant Breast Pathology
20.1. Role of Locoregional Treatment within a Patient-Based Multimodal Effort
20.1.1. Pre-Therapeutic Diagnostic Assessment and Strategy
20.1.2. Importance of Neoadjuvant Therapy
20.1.3. Importance of Inflammation: Healing Reaction
20.1.4. R0 Resection, Residual Disease and Therapeutic Consolidation Surgical
20.1.5. Pre and Perioperative Care
20.1.5.1. Antibiotic Prophylaxis
20.1.5.2. Thromboembolic Prophylaxis
20.1.5.3. MRSA Screening
20.1.5.4. Position in the Operating Room
20.1.5.5. Locoregional Analgesia
20.1.5.6. Nursing Care
20.1.6. Types of Surgical Procedure in Breast Cancer Selection Criteria
20.2. Conservative Breast Surgery: Fundamentals and Lumpectomy
20.2.1. Indications
20.2.2. Oncologic Principles
20.2.3. Plastic Principles
20.2.4. Guided Surgery
20.2.4.1. Wire
20.2.4.2. Markers
20.2.4.3. Isotopic (ROLL)
20.2.4.4. Seeds
20.2.5. Tumorectomy
20.2.5.1. Lymph Node Involvement
20.2.5.2. Incisions
20.2.5.3. Drainages
20.3. Conservative Breast Surgery: Oncoplastic Surgery
20.3.1. Foundations, Pioneers and History
20.3.2. Oncoplastic Procedures Quadrant by Quadrant
20.3.3. Oncoplastic Procedures Divided into Central Breast, Mid Breast; Social Breast and Peripheral Breast
20.3.4. Tubular Breasts and Breast Cancer
20.4. Reduction Mamoplasties and Breast Cancer
20.4.1. Indications
20.4.2. Types
20.5. Reduction Mammoplasties Quadrant by Quadrant
20.5.1. Contralateral Breast Symmetrization Mammoplasty
20.6. Mastectomy
20.6.1. Modified Radical Mastectomy Current Status
20.6.1.1. Description of the Modified Radical Mastectomy in the Current Day: Indications and Alternatives
20.6.1.2. Other Radical Mastectomies
20.6.2. Skin and CAP Conservative Mastectomy
20.6.3. Skin-Sparing Mastectomy
20.6.4. Reconstructive Aspects of Conservative Mastectomies
20.6.4.1. Prosthesis, Meshes and Matrices
20.6.4.2. Autologous Tissues
20.6.4.3. Immediate Reconstruction - Deferred
20.7. Stage IV Surgery, Recurrence and Metastases
20.7.1. When and How to Operate on a Metstatic Breast Cancer
20.7.2. Role of Surgery in Locoregional Recurrence, Within a Multidisciplinary Effort
20.7.3. Role of Surgery in Locoregional Palliation Within a Multidisciplinary Effort
20.7.4. Surgery in Locally Advanced Cancer
20.7.5. Electrochemotherapy
20.8. Lymphatic Surgery in Breast Cancer Significance and Importance
20.8.1. Importance of Preoperative Axillary Diagnosis and Marking
20.9. Selective Sentinel Node Biopsy
20.10. Surgical Management of the Axilla Postneadjuvancy
Module 21. Plastic and Reconstructive Surgery
21.1. Augmentation Mammoplasty
21.1.1. In Benign Pathology
21.1.2. In Symmetrization Augmentation Mammoplasty vs. Contralateral Glandectomy and Reconstruction
21.1.3. In Reparation of Sequelae of Conservative Surgery Local Flaps
21.2. Reduction Mammoplasty and Mastopexy
21.3. Breast Reconstruction: Immediate, Deferred and Immediate-Deferred
21.3.1. Radiological and Surgical Anatomy of the Breast Reconstruction
21.3.2. Preoperative Vascular Map
21.4. Prosthetic Reconstruction: Indications, Modes and Techniques
21.5. Pedicled Autologous Flaps
21.5.1. Local: Thoracodorsal Flap
21.5.2. Distance Broad Dorsal
21.5.2.2. TRAM Flap
21.6. Free Autologous Flaps
21.6.1. DIEP
21.6.2. Gracilis
21.6.3. Glute
21.6.4. Miscellaneous
21.6.5. CAP Reconstruction. Postoperative Management of Reconstructive Surgery
21.7. Sequelae Surgery
21.8. Sequelae of Conservative Breast Surgery and its Treatment
21.9. Scar Management
21.10. Lymphedema Surgery
21.10.1. Axillary Reverse Map
21.10.2. Surgical Management of Established Lymphedema
Module 22. Systemic Therapy in Breast Cancer
22.1. Cellular Cycle, Oncogenesis and Pharmacogenomics in Breast Cancer
22.2. Pharmokinetics and Tumor Response
22.3. Hormone Therapy
22.3.1. Basics of Hormone Therapy
22.3.2. Drugs Used
22.3.2.1. Selective Estrogen Receptor Modulators
22.3.2.2. GnRH Analogs
22.3.2.3. Aromatase Inhibitors
22.3.2.4. Antiestrogens
22.3.2.5. Antiprogestorens
22.3.2.6. Antiandrógenos
22.3.3. Prophylactic
22.3.3.1. Indications
22.3.3.2. Drugs Used
22.3.3.2.1. Tamoxifen
22.3.3.2.2. Raloxifen
22.3.3.2.3. Others
22.3.3.2.3.1. Retinoids
22.3.3.2.3.2. Cycloxygenase Inhibitors
22.3.3.2.3.3. Phytoestrogens
22.3.3.2.3.4. Statins
22.3.3.2.3.5. Tibolone
22.3.3.2.3.6. LHRH Analogs
22.3.3.2.3.7. Bisphosphonates
22.3.3.2.3.8. Calcium
22.3.3.2.3.9. Selenium
22.3.3.2.3.10. Vitamin D and E
22.3.3.2.3.11. Lapatinib
22.3.3.2.3.12. Metformina
22.3.4. Adjuvant
22.3.4.1. Indications
22.3.4.2. Duration
22.3.4.3. Early Disease
22.3.4.3.1. Tamoxifen
22.3.4.3.2. Aromatase Inhibitors
22.3.4.3.3. LHRH Analogs
22.3.4.4. Advanced Disease
22.3.4.4.1. Tamoxifen
22.3.4.4.2. Aromatase Inhibitors
22.3.4.4.3. LHRH Analogs and Surgical Castration
22.3.4.4.4. Cyclin 4-6 Inhibitors
22.3.5. Neoadjuvant
22.3.5.1. Indications
22.3.5.2. Schemes
22.3.5.3. Duration
22.4. Chemotherapy General Concepts
22.4.1. Basics of Chemotherapy
22.4.1.1. Importance of Dosis
22.4.1.2. Resistance to Chemotherapy
22.4.2. Drugs Used
22.5. First Line
22.5.1. Anthracyclines
22.5.2. Taxanes
22.5.3. Paclitaxel
22.5.4. Nab-Paclitaxel
22.5.5. Docetaxel
22.5.6. Others
22.5.6.1. Other Lines
22.6. Adjuvant
22.6.1. Early Disease
22.6.1.1. Schemes
22.6.2. Advanced Disease
22.6.2.1. Indications
22.6.2.2. Schemes
22.6.3. Neoadjuvant
22.6.3.1. Indications and Outlines
22.7. Target Therapies
22.7.1. Drugs Used
22.7.1.1. Anti Her2
22.7.1.2. Anti Angiogenics
22.7.1.3. mTor Inhibitors
22.7.1.4. Cyclin Inhibitor
22.7.1.5. Tirosin Kinasa Inhibitor
22.7.2. Adjuvant
22.7.2.1. Indications
22.7.2.2. Schemes
22.7.3. Neoadjuvant
22.7.3.1. Indications
22.7.3.2. Schemes
22.8. Immunotherapy
22.9. Support Therapies
22.9.1. Colony Stimulators
22.9.2. Antiemetics
22.9.3. Heart Protectors
22.9.4. Anti-alopecia
22.10. Complications
22.10.1. Infection in the Neutropenic Patient
22.10.2. Fungal and Viral Infections in Patients During Chemotherapy
22.10.3. Endocrine and Metabolic Complications in Patients During Chemotherapy
22.10.4. Emergency Oncology
Module 23. Radiotherapy
23.1. Basis of Radiotherapy
23.1.1. Radiobiology
23.1.2. Immunotherapy
23.2. Indications of Radiotherapy Treatment in the Breast
23.2.1. Radiotherapy after Conservative Treatment
23.2.2. Radiotherapy after Mastectomy
23.2.3. Radiation Therapy After Neoadjuvant Chemotherapy
23.2.4. Radiotherapy on Ganglionic Chains
23.3. Fractionation in Breast Cancer
23.3.1. Normofractionation
23.3.2. Hypofractionation
23.4. New Techniques
23.4.1. Partial Breast Irradiation: IORT, SBRT, External Beam Radiation Therapy
23.5. Radiotherapy in E IV patients: Oligometastatic Disease Palliative Radiotherapy
23.6. Reirradiation in Breast Cancer Radioprophylaxis Radiation Induced Breast Neoplasms
23.7. Radiotherapy and Quality of Life
23.7.1. Toxicity
23.7.2. Life Habits During Radiotherapy Treatment
23.8. Surgery Coordinated with Radiotherapy: Advantages
Module 24. Precision Oncology and Breast Cancer
24.1. Genomic Phenomena in the Progression of Breast Cancer
24.2. Genome, Transcriptome, Proteinome
24.3. Epigenetics
24.4. Germinal Line
24.5. Somatic Line
24.6. Fluid Biopsy
24.7. Risk signatures
24.8. Poor Responders
24.9. Relapse
24.10. Future
Develops solid skills through the use of real clinical cases, promoting clinical practice-based decision making”
Advanced Master's Degree in Integrative Gynecologic Oncology
Gynecologic cancer is a disease that requires specialized and updated care due to its complexity and constant evolution. At TECH Global University, a global leader in distance education, we have developed the Advanced Master's Degree in Integrative Gynecologic Oncology, a virtual training designed to provide health professionals with the knowledge and skills necessary for the diagnosis, treatment and follow-up of the different gynecologic neoplasms. This advanced master's Certificate in focuses on updating the most recent advances in early detection, surgical techniques, systemic therapies and management of side effects in the context of gynecologic oncology.
The program is designed to provide health professionals with the knowledge and skills necessary for the diagnosis, treatment and follow-up of the different gynecologic malignancies.
The Advanced Master's Degree program in Integrative Gynecologic Oncology at TECH Global University offers comprehensive training in the management of ovarian cancer, endometrial cancer, cervical cancer, vulvar cancer and other gynecologic tumors. Program participants will have the opportunity to interact with experts in the field, participate in clinical discussions and learn from real cases. In addition, clinical research topics will be addressed and the development of leadership skills in the field of gynecologic oncology will be promoted. Don't miss this opportunity and enhance your medical career with TECH Global University.
"







