University certificate
The world's largest faculty of medicine”
Why study at TECH?
Specialize in Gynecologic Oncology and stand out professionally in a booming sector. You will learn the latest developments in the industry from professionals"
TECH presents this Hybrid professional master’s degree program that will allow you to develop, with a real patient and in a hospital setting with state-of-the-art resources, your maximum potential and growth in the area of gynecologic oncology. You will approach patients with oncologic pathology by the hand of the best specialists, using the latest techniques based on scientific evidence, and achieving results previously difficult to ach ieve.
The social and emotional burden that gynecological cancer has on today's society means that scientific and professional interest in this discipline is on the rise. But advances in surgery and gynecologic oncology make it essential for specialists to maintain constant training in order to continue providing quality care. This Hybrid professional master’s degree program offers the opportunity to update knowledge in a practical way.
Gynecologic Oncology has undergone remarkable development in the past few years. Both specialties, gynecology and oncology, face increasingly complex challenges associated with the development of diagnostic and therapeutic techniques. Not only this, but also technological and IT innovations, and the use of biomaterials and new, much more conservative, surgical procedures.
These new developments force the specialist to constantly update his knowledge, to study the available evidence and to develop new competencies, which allow him to keep up with the technological and social changes to improve the health of patients.
This program will allow the specialist to access this knowledge in a practical way, without renouncing scientific rigor, adapting the training process to their personal and professional needs. In this way, he will integrate into his daily clinical practice the latest advances in Gynecologic Oncology, marking a before and after in his professional career.
You will access 10 exclusive high-quality Masterclasses, prepared by an internationally recognized expert. Update yourself with #TECH in Gynecologic Oncology!”
This Hybrid professional master’s degree in Gynecologic Oncology contains the most complete and up-to-date scientific program on the market. The most important features include:
- Development of more than 100 clinical cases, recorded with POV (Point Of View) systems from different angles, presented by experts in Gynecology and other specialties
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- Presentation of practical workshops on procedures and techniques
- An algorithm-based interactive learning system for decision-making in the clinical situations presented throughout the course
- Action protocols and clinical practice guidelines, which cover the most important latest developments in this specialist area
- Special emphasis on test-based medicine and research methodologies in surgical procedures
- All of this will be complemented by theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
- In addition, you will be able to carry out a clinical internship in one of the best hospitals in the world
The scientific evidence on which this program is based increases the quality of medical and surgical practice. Staying current is key to providing better patient care"
In this Hybrid professional master’s degree proposal, of a professionalizing nature and blended learning modality, the program is aimed at updating medical professionals who perform their functions in the Gynecologic Oncology unit, and who require a high level of qualification. The contents are based on the latest scientific evidence, and oriented in a didactic way to integrate theoretical knowledge into medical practice, and the theoretical-practical elements will facilitate the updating of knowledge and will allow decision making in patient management.
Thanks to their multimedia content developed with the latest educational technology, they will allow medical professional a situated and contextual learning, that is, a simulated environment that will provide an immersive learning programmed to train in real situations. This program is designed around Problem-Based Learning, whereby the professional must try to solve the different professional practice situations that arise throughout the program. For this reason, you will be assisted by an innovative, interactive video system created by renowned and experienced experts in the field of Intensive Care units who also have extensive teaching experience.
This highly scientifically rigorous training provides immersive learning programmed to train for real-life situations"

Update your knowledge through the Hybrid professional master’s degree in Gynecologic Oncology, in a practical way and adapted to your needs"
Teaching Planning
This innovative training model has been designed so that today's professionals can acquire theoretical knowledge at their own pace and without complications, and then test it in an on-site stage in one of the most prestigious clinical centers specialized in Gynecologic Oncology. For this reason, a curriculum has been established whose modules offer a broad perspective of the different types of cancer, their analysis, diagnoses, treatments and approaches from a global point of view for the sake of their application at an international level. In 15 study modules and an internship, students will expand their knowledge, which will allow them to stand out in their work environment.

A unique program featuring the most cutting-edge curriculum in Gynecologic Oncology, which you will study alongside leading experts”
Module 1. Biological Basis of Cancer
1.1. Cell Growth Regulation
1.2. Carcinogenesis and Carcinogens
1.3. Genetics of Cancer
1.4. Mechanisms of Apoptosis and Programmed Cell Death
1.5. Molecular Mechanisms of Cancer Production and Metastasis
1.6. Origin of Genetic Alterations
1.7. Epigenetic Changes and Oncogenes
1.8. Angiogenesis
Module 2. Basis of Chemotherapy Treatment, Adverse Effects and New Therapies
2.1. Introduction
2.2. Justification for the Use of Chemotherapy
2.3. Development of Cancer and the Influence of Chemotherapy
2.3.1. Tumor Growth
2.3.2. Cellular Cycle
2.3.3. Specific Drugs for each of the Cellular Phases
2.4. Factors that Influence Treatment
2.4.1. Tumor Characteristics
2.4.2. Patient Tolerence
2.4.3. Treatment Objectives
2.4.4. Pharmacological Factors and Administration Routes
2.5. Principles of Resistance to Drugs
2.6. Combined Therapies
2.7. Treatment or Dosis Adjustments
2.8. Drug Toxicity
2.9. General Management of Secondary Effects and Complications of Chemotherapy
2.10. Antineoplastic Agents in Gynecology
2.10.1. Alkylating Agents
2.10.2. Antibiotics
2.10.3. Anti-metabolites
2.10.4. Plant Alkaloids
2.10.5. Topoisomerase 1 Inhibitors
2.10.6. Anti-Angiogenic Drugs
2.10.7. PARP Inhibitors
2.10.8. Tyrosine Kinase Inhibitors
2.10.9. Other Drugs
2.11. Future Indications
Module 3. Endometrial Cancer I
3.1. Epidemiology and Etiopathogenesis
3.2. Precancerous Lesions
3.3. Hereditary-Familial Carcinoma
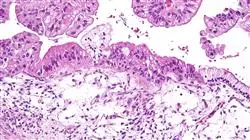
3.4. Pathological Anatomy and Different Types of Tumors
3.5. Diagnostic Process
3.6. Imaging Tests, Tumor Markers and Possible Screening
3.7. Molecular Diagnostic Tests
3.8. FIGO Clasiffication and Others
Module 4. Endometrial Cancer II
4.1. Introduction
4.2. General Aspects of Surgical Treatment
4.3. Low Risk Tumors (Stage I, Grade 1)
4.4. High Risk Tumors (Grade 2-3, Serous or Clear Cells)
4.5. Laparotomy vs. Laparoscopy
4.6. Introduction of Robotic Surgery
4.7. Surgical Technique for High Risk Tumors
4.8. Adjuvant Treatment
4.8.1. Observation without Additional Treatment
4.8.1.1. Low Risk, Early Stage, Low Grade
4.8.2. Adjuvant Radiotherapy
4.8.2.1. Early Stage, Intermediate and High Risk
4.8.2.2. Advanced Stages
4.8.3. Adjuvant Chemotherapy
4.8.4. Peculiarities of Serous Tumors and Clear Cells
4.9. Hormonal Treatment
4.10. Recurrent Endometrial Cancer
4.10.1. Surgical Management
4.10.2. Radiotherapy
4.10.3. Chemotherapy
4.11. Follow-up Treatment of Endometrial Cancer
4.12. Prognosis
Module 5. Cervical Cancer I
5.1. Epidemiology and Etiopathogenesis of the Disease
5.2. Precancerous Lesions and the Evolutionary Process
5.3. Risk Factors for Contracting the Disease
5.4. Notions about Cervical Pathology and HPV
5.5. Normal Colposcopy and Vulvoscopy
5.6. Abnormal Colposcopy and Vulvoscopy
5.7. Cervical Cancer Screening
5.8. Hereditary-Familial Carcinoma
5.9. Forms of Presentation in Anatomic Pathology
5.10. Diagnostic Process: Imaging Tests and Tumor Markers
5.11. Role of New Technologies such as PET-CT
5.12. FIGO and TNM Classification in Cervical Carcinoma
Module 6. Cervical Cancer II
6.1. Treatment of Cervical Intraepithelial Neoplasia (CIN)
6.1.1. CIN Surgery
6.1.2. CIN Immunotherapy
6.2. Invasive Treatment of Cervical Cancer
6.2.1. Radical Hysterectomy with Nerve Preservation
6.2.2. Less Radical Hysterectomy
6.2.3. Radical Endoscopic Hysterectomy
6.2.4. Selective Sentinel Node Biopsy
6.2.5. Para-aortic Advanced Stage Lymphadenectomy Staging
6.3. Radiotherapy and Chemotherapy
6.3.1. Concurrent Chemoradiotherapy
6.3.2. Enhanced Radiation Therapy Treatment Modalities
6.3.3. Chemotherapy Modalities in Concurrent Treatment
6.3.4. Preoperative Chemoradiotherapy
6.3.5. Adjuvant Therapy after a Radical Hysterectomy
6.3.6. Neoadjuvant Chemotherapy
6.3.7. Adjuvant Therapy after Neoadjuvant and Previous Surgery
6.4. Treatment of Metastasis, Recurrent or Persistent Disease
6.4.1. Surgical Management
6.4.2. Chemotherapy
6.5. Management of Cervical Adenocarcinoma
6.5.1. Adenocarcinoma in Situ (AIS)
6.5.2. Comparison Between Squamous Cell Carcinomas and Adenocarcinomas
6.5.3. Surgery vs. Radiotherapy in Invasive Adenocarcinoma
6.5.4. Chemotherapy
6.6. Monitoring
Module 7. Ovarian Cancer I
7.1. Epidemiology of Ovarian and Fallopian Tube Cancer
7.2. Etiopathogenesis and tubal origin, new trends
7.3. Precancerous Lesions in the Fallopian Tubes
7.4. Ovarian Cancer Screening
7.5. Hereditary-Familial Carcinoma and How to Evaluate It
7.6. Histological Forms and Pathological Anatomy
7.7. Diagnostic Process
7.7.1. Clinical Symptoms
7.7.2. Ultrasound
7.7.3. Computerized Tomography
7.7.4. Magnetic Resonance
7.7.5. Positron Emission Tomography
7.8. Serum Tumor Markers
7.8.1. CA125
7.8.2. HE4
7.8.3. CA19.9.
7.8.4. CEA
7.8.5. Other Markers
7.9. FIGO Classification of the Disease
Module 8. Ovarian Cancer II
8.1. General Surgical Treatment
8.2. Complete Cytoreduction and Primary Debulking
8.3. Neoadjuvant Treatment and When to Opt for It
8.4. Interval and Second Look Treatments
8.5. Adjuvant Therapy: Carboplatin-Taxol and Other Options
8.6. Radiotherapy: What Role Does it Play?
8.7. Hormonal Therapy Possibilities in Ovarian Cancer
8.8. Prognosis and Disease-Free Interval
8.9. Monitoring and Treatment of Relapses
8.10. Controversies in the Management of Ovarian Cancer
8.11. Peritoneal Carcinomas Hyperthermic Therapy
8.12. Intraperitoneal Chemotherapy, Indications and Results
Module 9. Vulvar Cancer I
9.1. Epidemiology and Relationship with HPV
9.2. Etiopathogenesis and Precancerous Lesions
9.3. VIN I, II, III VAIN and Other Lesions
9.4. Vulvar Cancer Screening
9.5. Hereditary-Familial Carcinoma
9.6. Pathological Anatomy, Histological Types
9.7. Imaging Tests and Extension Study
9.8. Tumor Markers: SCC
Module 10. Vulvar Cancer II
10.1. Introduction
10.2. Vulvar Paget’s Disease
10.2.1. General Aspects
10.2.2. Paget’s Disease Type 1
10.2.2.1. Prevalence
10.2.2.2. Clinical Characteristics
10.2.2.3. Diagnosis
10.2.2.4. Treatment
10.2.3. Paget’s Disease Type 2 and 3
10.3. Invasive Paget’s Disease
10.3.1. General Aspects
10.3.2. Prognosis
10.4. Invasive Vulva Carcinoma
10.4.1. Squamous Cell Carcinoma
10.4.2. Clinical Characteristics
10.4.3. Diagnosis
10.4.4. Dissemination Pathways
10.4.5. Staging
10.4.6. Treatment
10.4.6.1. Primary Lesion Management
10.4.6.2. Local Control after Primary Surgical Treatment
10.4.6.3. Management of Ganglionic Chains
10.4.6.4. Post-Operative Care
10.4.6.4.1. Early postoperative complications
10.4.6.4.2. Late Postoperative Complications
10.4.6.5. Use of Sentinel Lymph Node
10.4.6.5.1. Advanced Disease
10.4.6.5.2. General Aspects
10.4.6.5.3. Management of Ganglionic Chains
10.4.6.5.4. Management of Primary Tumor
10.4.6.5.4.1. Surgery
10.4.6.5.4.2. Radiotherapy
10.4.6.5.4.3. Chemotherapy
10.4.6.6. Role of radiotherapy in vulvar cancer
10.4.7. Recurrent Vulvar Cancer
10.4.8. Prognosis
10.4.9. Monitoring
10.5. Vulva Melanoma
10.5.1. Introduction
10.5.2. Clinical Characteristics
10.5.3. Pathologic Anatomy
10.5.4. Staging
10.5.5. Treatment
10.5.5.1. Primary Lesion Management
10.5.5.2. Management of Ganglionic Chains
10.5.6. Prognosis
10.6. Carcinoma of Bartholin’s Gland
10.6.1. General Aspects
10.6.2. Treatment
10.6.3. Prognosis
10.7. Basal Cell Carcinoma
10.8. Verrucous Carcinoma
10.9. Vulva Sarcoma
10.9.1. Introduction
10.9.2. Leiomyosarcoma
10.9.3. Epithelioid Sarcoma
10.9.4. Rhabdomyosarcoma
10.9.5. Merkel Cells Carcinoma
Module 11. Uterine Sarcoma I
11.1. Introduction
11.2. Epidemiology
11.2.1. Incidence
11.2.2. Age
11.2.3. Histological Distribution
11.2.4. Racial Distribution
11.3. Risk Factors
11.3.1. Heritage
11.3.2. Hormone Therapy
11.3.3. Radiation Exposure
11.4. Pathologic Anatomy
11.4.1. Leiomyosarcoma
11.4.2. STUMP
11.4.3. Benign Metastasizing Leiomyoma
11.4.4. Carcinosarcoma
11.4.5. Endometrial Stromal Neoplasms
11.4.6. Stromal Nodule
11.4.7. Endometrial Stromal Sarcoma
11.4.8. Mullerian Adenosarcoma
11.5. Clinical Manifestations
11.6. Imaging Tests
11.6.1. Magnetic Resonance
11.6.2. Tumor Markers
11.7. FIGO Staging
11.8. Conclusions
Module 12. Uterine Sarcoma II
12.1. Introduction
12.2. Uterine Leiomyosarcoma
12.2.1. Early Stages
12.2.1.1. Surgery
12.2.1.2. Adjuvant Radiotherapy
12.2.1.3. Chemotherapy
12.2.2. Recurrent or Metastatic Disease
12.2.2.1. Surgery
12.2.2.2. Chemotherapy
12.2.2.3. Hormone Therapy
12.2.3. Prognostic Factors
12.3. Endometrial Stromal Sarcoma
12.3.1. Early Stages
12.3.1.1. Surgery
12.3.1.2. Pelvic Radiotherapy
12.3.1.3. Hormone Therapy
12.3.2. Recurrent or Metastatic Disease
12.3.2.1. Surgery
12.3.2.2. Chemotherapy or Radiotherapy
12.3.3. Prognostic Factors
12.4. Undifferentiated Endometrial Sarcoma
12.4.1. Early Stages
12.4.1.1. Surgery
12.4.1.2. Adjuvant Radiotherapy
12.4.1.3. Chemotherapy
12.4.2. Recurrent or Metastatic Disease
12.4.2.1. Surgery
12.4.2.2. Chemotherapy or Radiotherapy
12.4.3. Prognostic Factors
12.5. Conclusions
Module 13. Fertility Preservation
13.1. Indications of Fertility Preservation
13.2. Gametes Preservation
13.3. Role of Assisted Reproduction Techniques
13.4. Conservative Surgical Treatment
13.5. Oncological Prognosis after Fertility Conservation
13.6. Reproductive Results
13.7. Dealing with Pregnant Women with Gynecologic Cancer
13.8. New research paths and literature updates
13.9. Conservation of Ovarian Tissue
13.10. Uterine and Gonadal Tissue Transplantation
Module 14. Uncommon Gynecologic Tumors
14.1. Vagina Cancer
14.1.1. Introduction
14.1.2. Clinical Manifestations
14.1.3. Diagnosis
14.1.4. Pathologic Anatomy
14.1.4.1. Squamous Carcinoma
14.1.4.2. Adenocarcinoma
14.1.4.3. Sarcoma
14.1.4.4. Melanoma
14.1.5. Tumor Staging
14.1.6. Treatment of Disease
14.1.6.1. Surgery
14.1.6.2. Radiotherapy
14.1.6.3. Treatment Complications
14.1.7. Monitoring
14.1.8. Prognosis
14.2. Gestational Trophoblastic Disease
14.2.1. Introduction and Epidemiology
14.2.2. Clinical Forms
14.2.2.1. Hydatidiform Mole
14.2.2.1.1. Complete Hydatidiform Mole
14.2.2.1.2. Partial Hydatidiform Mole
14.2.2.2. Gestational Trophoblastic Neoplasm
14.2.2.2.1. After Molar Pregnancy
14.2.2.2.1.1. Persistent Gestational Trophoblastic Neoplasm
14.2.2.2.2. After Non-Molar Pregnancy
14.2.2.2.2.1. Choriocarcinoma
14.2.2.2.2.2. Placental Site Trophoblastic Tumor
14.2.3. Diagnosis
14.2.3.1. Human Chorionic Gonadotropin
14.2.3.2. Ultrasound Study
14.2.3.2.1. Complete Mole
14.2.3.2.2. Partial Mole
14.2.3.2.3. Invasive Mole
14.2.3.2.4. Choriocarcinoma and Placental Site Tumor
14.2.3.3. Other Imaging Techniques
14.2.4. Pathologic Anatomy
14.2.4.1. Hydatidiform Mole
14.2.4.1.1. Complete Mole
14.2.4.1.2. Partial Mole
14.2.4.2. Invasive Mole
14.2.4.3. Choriocarcinoma
14.2.4.4. Placental Site Trophoblastic Tumor
14.2.4.5. Epithelioid Trophoblastic Tumor
14.2.5. Staging
14.2.6. Treatment
14.2.6.1. Chemotherapy
14.2.6.1.1. Low Risk Disease
14.2.6.1.2. High Risk Disease and Metastasis
14.2.6.1.3. Chemoresistant Disease
14.2.6.2. Surgery
14.2.6.2.1. Molar Evacuation
14.2.6.2.2. Hysterectomy
14.2.6.2.3. Myometrial Resection
14.2.6.2.4. Pulmonary Resection
14.2.6.2.5. Craniotomy
14.2.6.2.6. Other Surgical Procedures
14.2.6.2.7. Selective Arterial Embolization
14.2.7. Post-Treatment Monitoring
14.2.7.1. Monitoring after Molar Evacuation
14.2.7.2. Monitoring after Gestational Neoplasm Treatment
14.2.8. Prognosis
14.3. Metastatic Tumor in the Genital Tract
14.3.1. Introduction
14.3.2. Clinical Manifestations
14.3.2.1. Secondary Tumors in the Uterine Body or Cervix
14.3.2.2.1. From Genital or Pelvic Organs
14.3.2.2.2. From Extragenital or Pelvic Organs
14.3.2.2. Secondary Tumors in the Vagina
14.3.2.3. Secondary Tumors on the Vulva
14.3.2.4. Secondary Tumors in the Ovaries
14.3.3. Diagnosis
14.3.4. Pathologic Anatomy
14.3.4.1. Gastrointestinal Tumors
14.3.4.1.1. Metastasis of Intestinal Cancer
14.3.4.1.2. Krukenberg Tumor
14.3.4.2. Ovarian Lymphona
14.3.5. Treatment and Prognosis
14.4. Neuroendocrine Tumors
14.4.1. Introduction
14.4.2. Pathologic Anatomy
14.4.2.1. Well-Differentiated Tumors
14.4.2.2. Poorly-Differentiated Tumors
14.4.3. Clinical Manifestations and Diagnosis
14.4.3.1. Small Cell Tumor in the Vulva and Vagina
14.4.3.2. Small Cell Tumor in the Uterus
14.4.3.3. Neuroendocrine Tumors in the Cervix
14.4.3.3.1. Small Cell Neuroendocrine Carcinoma
14.4.3.3.2. Carcinoma neuroendocrino células grandes
14.4.3.4. Ovarian, Fallopian Tube and Wide Ligament Tumor
14.4.3.4.1. Ovarian Carcinoid
14.4.3.4.1.1. Insular Carcinoid
14.4.3.4.1.2. Trabecular Carcinoid
14.4.3.4.1.3. Mucinous Carcinoid
14.4.3.4.1.4. Strumal Carcinoid
14.4.3.4.2. Small Cell Lung Type
14.4.3.4.3. Undifferentiated Non-Small Cell Carcinoma
14.4.4. Treatment
14.4.5. Monitoring
14.4.6. Prognosis
14.5. Tumors of the Recto-Vaginal Septum
Module 15. Palliative Care and Nutrition
15.1. Introduction
15.1.1. Symptomology Associated with Gynecologic Tumors
15.2. Pain
15.3. Gastrointestinal Symptoms
15.3.1. Diarrhea
15.3.2. Constipation
15.3.3. Malignant Intestinal Obstruction
15.3.3.1. Conservative Treatment
15.3.3.2. Surgical Management
15.4. Ascites
15.5. Respiratory symptoms
15.5.1. Pleural Effusion
15.6. Edema
15.7. Anorexia and Weight Loss
15.8. Deep Vein Thrombosis
15.9. Pelvic Disease Progression
15.9.1. Vaginal Bleeding
15.9.2. Fistulas
15.10. Palliative Pelvic Exenteration
15.11. Metastasis of Other Organs
15.11.1. Liver
15.11.2. Brain
15.11.3. Bone
15.11.3.1. Hypercalcemia
15.12. Anxiety and Depression
15.13. Dying Patient Care

A unique, key and decisive update experience to boost your professional development”
Hybrid Professional Master's Degree in Gynecologic Oncology
At TECH Global University, we offer you the opportunity to specialize in the field of gynecologic oncology through our Hybrid Professional Master's Degree in Gynecologic Oncology. This postgraduate program is designed for health professionals who wish to acquire the knowledge and skills necessary to provide specialized care to patients with gynecologic oncologic diseases. Our program combines the convenience of blended learning with the academic excellence that characterizes us. Here, we will provide you with comprehensive training in the diagnosis and treatment of gynecologic oncologic diseases, including ovarian cancer, endometrial cancer, cervical cancer and vulvar cancer, among others. You will learn the latest surgical techniques and procedures, as well as the comprehensive management of the oncologic patient, including emotional and psychological support. Our program will prepare you to face the clinical and scientific challenges of gynecologic oncology in daily practice, enhancing your professional profile and expanding your career opportunities in this ever-evolving field.
Study a postgraduate degree at the best medical school
One of the advantages of our Hybrid Professional Master's Degree in Gynecologic Oncology is the flexibility it offers. You will be able to access the contents of the program through our online platform, which will allow you to study at your own pace and adapt the lessons to your schedule and availability. In addition, you will have face-to-face classes with experts in the field of gynecologic oncology, where you will be able to interact with other professionals and expand your knowledge through clinical cases and group discussions. At TECH Global University, we are committed to your professional growth and we offer you a Semipresential postgraduate program that will allow you to acquire the knowledge and skills necessary to excel in the field of gynecologic oncology. Don't wait any longer, enroll in our program and boost your career in the medical field!