University certificate
The world's largest faculty of medicine”
Description
This Postgraduate diploma contains the most complete and up-to-date scientific program on the market"
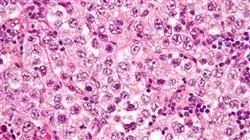
Research in the fields of gynecology and urology is extremely important for increasing the survival rates of people suffering from tumors in these areas. However, technological development is equally important, as the tools for treating these diseases are improving all the time.
Advances in radiation oncology in recent decades have increased the chances of curing certain types of cancer, as well as reducing the possible side effects and complications caused by radiation in patients.
Radiation oncologists must be in constant contact with this type of technology in order to provide the best care for their patients. For this reason, it is especially important that these professionals are constantly recycling and updating their knowledge through training courses such as this one, in which they will learn the main developments in the subject. In this case there is a special emphasis on gynecologic and urologic tumors.
In this Postgraduate diploma, the healthcare professional will delve into the field of radiotherapy treatment, focusing on the most effective procedures for different types of cancer. This will allow them to gain knowledge which is adapted to the new advances and study a more comprehensive training course to develop their professional work in the most effective way possible.
Increase your clinical skills through this Postgraduate diploma program in Radiotherapy Treatment of Gynecologic and Urologic Tumors"
This Postgraduate diploma in Radiotherapy Treatment of Gynecologic and Urologic Tumors contains the most comprehensive and up-to-date scientific program on the market. The most important features of the program include:
- Clinical cases presented by experts in Radiotherapy Treatment of Gynecologic and Urologic Tumors
- The graphic, schematic and eminently practical contents of which they are composed provide scientific and practical information on the disciplines that are essential for professional practice
- Diagnostic-therapeutic developments in assessment, diagnosis and intervention in gynecologic and urologic tumors
- It contains practical exercises where the self-evaluation process can be carried out to improve learning
- Clinical and diagnostic imaging and testing iconography
- Algorithm-based interactive learning system for decision-making in the presented clinical situations
- With special emphasis on evidence-based medicine and research methodologies in gynecologic and urologic tumors
- All of this will be complemented by theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive training program designed to train in real situations”
The teaching staff includes professionals from the field of Radiotherapy Treatment of Gynecologic and Urologic Tumors, who bring their experience to this training program, as well as renowned specialists from leading scientific societies.
The multimedia content developed with the latest educational technology will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive training program to train in real situations.
This program is designed around Problem Based Learning, whereby the physician must try to solve the different professional practice situations that arise during the course. For this purpose, the physician will be assisted by an innovative interactive video system developed by renowned experts in the field of Radiotherapy Treatment of Gynecologic and Urologic Tumors with extensive teaching experience.
Train with us and update you knowledge in order to offer more efficient and personalized care to your patients"

Don't miss the opportunity and get up to date on advances in the treatment of gynecologic and urologic tumors in order to incorporate them into your daily medical practice"
Syllabus
The structure of the content has been designed by the best professionals in radiation oncology who work in centers of national reference. These experts are aware of the need for training in the world of medicine in order to advance in radiotherapy treatment of gynecologic and urologic tumors. That is why they offer this quality training, adapted to new educational technologies, so that health professionals can provide the best medical care, adapting it to the needs of their patients.

It includes clinical cases to bring the program content as close as possible to the reality of medical practice”
Module 1. Basis of Radiotherapy Treatment Radiobiology
1.1. Biological Effects of Ionizing Radiations
1.1.1. DNA Damage
1.1.2. Non-Clonal Effects
1.2. Dose Fractionation
1.2.1. Linear-Quadratic Model
1.2.2. Time Factor in Radiotherapy
1.2.3. Altered Subdivisions
1.3. Oxygen Effect and Tumor Hypoxia
1.4. Radiobiology of Brachytherapy
1.5. Effects of Irradiation on Healthy Tissues
1.6. Combination of Irradiation with Drugs
1.7. Predictive Assays of Response to Radiotherapy
1.8. Radiobiology of Re-Irradiation
1.9. Effects of Irradiation on the Embryo and Fetus
1.10. Radiation-Induced Carcinogenesis
Module 2. Update on Radiotherapy Treatment of Gynecologic Tumors
2.1. Endometrial Cancer
2.1.1. Epidemiological Aspects
2.1.2. Risk Factors
2.1.3. Anatomy Recap
2.1.4. Histological Type
2.1.5. Dissemination Pathways
2.1.6. Classification
2.1.7. Prognostic Factors
2.1.8. Surgical Treatment
2.1.9. Adjuvant Early Stage Radiotherapy Treatment
2.1.10. Advanced Disease
2.1.11. Local, Regional, Distant Relapse
2.1.12. Follow up
2.2. Uterine Sarcomas
2.2.1. Epidemiological Aspects
2.2.2. Risk Factors
2.2.3. Anatomy Recap
2.2.4. Histological Type
2.2.5. Dissemination Pathways
2.2.6. Classification
2.2.7. Prognostic Factors
2.2.8. Surgical Treatment
2.2.9. Adjuvant Early Stage Radiotherapy Treatment
2.2.10. Advanced Disease
2.2.11. Local, Regional, Distant Relapse
2.2.12. Follow up
2.3. Cervical Cancer
2.3.1. Epidemiological Aspects
2.3.2. Risk Factors
2.3.3. Anatomy Recap
2.3.4. Histological Type
2.3.5. Dissemination Pathways
2.3.6. Classification
2.3.7. Prognostic Factors
2.3.8. Surgical Treatment
2.3.9. Adjuvant Early Stage Radiotherapy Treatment
2.3.10. Advanced Disease
2.3.11. Local, Regional, Distant Relapse
2.3.12. Follow up
2.4. Vulvar Cancer
2.4.1. Epidemiological Aspects
2.4.2. Risk Factors
2.4.3. Anatomy Recap
2.4.4. Histological Type
2.4.5. Dissemination Pathways
2.4.6. Classification
2.4.7. Prognostic Factors
2.4.8. Surgical Treatment
2.4.9. Adjuvant Early Stage Radiotherapy Treatment
2.4.10. Advanced Disease
2.4.11. Local, Regional, Distant Relapse
2.4.12. Follow up
2.5. Vagina Cancer
2.5.1. Epidemiological Aspects
2.5.2. Risk Factors
2.5.3. Anatomy Recap
2.5.4. Histological Type
2.5.5. Dissemination Pathways
2.5.6. Classification
2.5.7. Prognostic Factors
2.5.8. Surgical Treatment
2.5.9. Adjuvant Early Stage Radiotherapy Treatment
2.5.10. Advanced Disease
2.5.11. Local, Regional, Distant Relapse
2.5.12. Follow up
2.6. Fallopian Tube and Ovarian Cancer
2.6.1. Epidemiological Aspects
2.6.2. Risk Factors
2.6.3. Anatomy Recap
2.6.4. Histological Type
2.6.5. Dissemination Pathways
2.6.6. Classification
2.6.7. Prognostic Factors
2.6.8. Surgical Treatment
2.6.9. Adjuvant Early Stage Radiotherapy Treatment
2.6.10. Advanced Disease
2.6.11. Local, Regional, Distant Relapse
2.6.12. Follow up
Module 3. Update on Radiotherapeutic Treatment of Prostate and Other Urological Tumors
3.1. Prostate Cancer
3.1.1. Low Risk
3.1.2. Intermediate Risk
3.1.2.1. Definition of Intermediate Risk Prostate Cancer
3.1.2.2. Subclassification of Intermediate Risk Prostate Cancer
3.1.2.2.1. Importance of Gleason 7
3.1.2.3. Diagnosis and Extension Study
3.1.2.4. Treatment
3.1.2.4.1. Active Surveillance
3.1.2.4.2. Radical Prostatectomy
3.1.2.4.3. Radiotherapy Techniques and Requirements
3.1.2.4.3.1. Role of External Radiation Therapy
3.1.2.4.3.2. The Role of Brachytherapy
3.1.2.4.3.3. The Role of Stereotactic Body Radiotherapy SBRT
3.1.2.4.3.4. Combined Treatments
3.1.2.4.4. Hormone Therapy. When and How Much?
3.1.2.4.5. The Best Option for Each Patient
3.1.2.5. Follow up
3.1.2.6. Conclusions
3.1.3. High Risk
3.1.4. Local and/or Distant Relapse Treatment
3.1.4.1. Treatment of Local Relapse
3.1.4.1.1. After Prostatectomy
3.1.4.1.2. After Radiotherapy
3.1.4.1.2.1. Rescue Surgery
3.1.4.1.2.2. Rescue Cryotherapy
3.1.4.1.2.3. Rescue Brachytherapy
3.1.4.1.2.4. High Intensity Focused Ultrasound (HIFU)
3.1.4.1.2.5. Intermittent Hormone Rescue
3.1.4.2. Treatment of Distant Relapse
3.1.4.2.1. Metastatic Patient
3.1.4.2.2. Oligorecurrent Patient
3.1.4.2.2.1. Hormonal Treatment
3.1.4.2.2.2. Surgical Treatment
3.1.4.2.2.3. SBRT Treatment
3.2. Preoperative and Postoperative Radiotherapy in Bladder Cancer
3.2.1. Introduction
3.2.2. Preoperative Radiotherapy
3.2.2.1. Bibliographic Review
3.2.2.2. Indications
3.2.3. Postoperative Radiotherapy
3.2.3.1. Bibliographic Review
3.2.3.2. Indications
3.2.4. Organ Conservative Treatment
3.3. Testicular Tumors
3.3.1. Introduction
3.3.2. Histological Type
3.3.3. TNM Classification and Prognostic Groups
3.3.4. Germinal Tumors: Treatment According to Stage and Prognostic Group
3.3.4.1. Seminoma
3.3.4.2. Non-Seminoma
3.3.5. Toxicity of Chemotherapy and Radiotherapy
3.3.6. Secondary Neoplasms
3.3.7. Non-Germ Cell Tumours
3.4. Renal, Ureteral, and Urethral Tumors
3.4.1. Kidney Tumors
3.4.1.1. Clinical Presentation
3.4.1.2. Diagnosis
3.4.1.3. Localized Disease Treatment
3.4.1.4. Advanced Disease Treatment
3.4.2. Urethral Tumors
3.4.2.1. Clinical Presentation: Men vs. Women
3.4.2.2. Diagnosis
3.4.2.3. Treatment
3.4.3. Ureter and Renal Pelvis Tumors
3.4.3.1. Risk Factors
3.4.3.2. Presentation: Primary Tumor-Metastasis
3.4.3.3. Symptoms/Clinical
3.4.3.4. Diagnosis
3.4.3.5. Localized Disease Treatment
3.4.3.6. Advanced Disease Treatment
3.5. Penis Cancer
3.5.1. Adjuvant Treatment
3.5.2. Radical Treatment
3.6. Treatment of Adrenal Metastases
3.6.1. Introduction
3.6.2. Surgery
3.6.3. Stereotactic Body Radiotherapy (SBRT)
Module 4. Pain and Nutrition in Radiation Oncology
4.1. General Information on Oncologic Pain
4.1.1. Epidemiology
4.1.2. Prevalence
4.1.3. Impact of Pain
4.1.4. Multidimensional Concept of Cancer Pain
4.2. Characterization of Pain
4.2.1. Types of Oncologic Pain
4.2.2. Evaluation of Oncologic Pain
4.2.3. Prognosis of Pain
4.2.4. Classification
4.2.5. Diagnostic Algorithm
4.3. General Principles of Pharmacological Treatment
4.4. General Principles of Radiotherapy Treatment
4.4.1. External Radiotherapy
4.4.2. Dosages and Fractions
4.5. Bisphosphonates
4.6. Radiopharmaceuticals in the Management of Metastatic Bone Pain
4.7. Pain in Long-Term Survivors
4.8. Nutrition and Cancer
4.8.1. Concept of Malnutrition
4.8.2. Prevalence of Malnutrition
4.8.3. Causes and Consequences of Malnutrition in Oncology Patients
4.8.4. Mortality and Survival
4.8.5. Nutritional Risk Factors in Oncology Patients
4.8.6. Objectives of Nutritional Support
4.9. Cachexia
4.10. Initial Nutritional Assessment in a Radiation Oncology Service
4.10.1. Diagnostic Algorithm
4.10.2. Specific Treatment
4.10.3. General Dietary Recommendations
4.10.4. Specific Individualized Recommendations
4.11. Nutritional Assessment During Monitoring in a Radiation Oncology Service

Don’t miss this opportunity to train with us and acquire the necessary skills to give your all in your job”
Postgraduate Diploma in Radiotherapy Treatment of Gynecologic and Urologic Tumors
Cancer is one of the main causes of mortality worldwide, and its treatment is one of the greatest challenges facing medicine today. Advances in radiation oncology in recent decades have increased survival rates in certain types of cancer, as well as decreased possible side effects and radiation complications in patients. TECH has designed the Postgraduate Diploma in Radiotherapy Treatment of Gynecological and Urological Tumors, a program that will allow you to delve into the latest advances in radiotherapy treatment and radiobiology, focusing on the most effective procedures for each type of cancer.
Get trained 100% online in the radiotherapeutic treatment of gynecological and urological cancers.
The advanced methodology of this Postgraduate Diploma, as well as its outstanding teaching staff, will provide you with the fundamental bases to offer a more effective and safe care to your patients, delving into pre- and post-operative radiotherapy treatments, as well as pain management and nutritional assessment in radiation oncology. In addition to this, you will remain in constant training to be at the forefront of the latest technologies in the treatment of Gynecologic and Urologic Tumors.







