University certificate
The world's largest faculty of nursing”
Why study at TECH?
Update yourself with this top level Hybrid Master about the most modern protocols and procedures included in the professional field of nursing for the management of patients with pain"
The scientific contributions related to Pain Management have been significant in recent years. Through various researches, therapeutic methods such as gene treatments, neurostimulation or neurolytic blocks have appeared. At the same time, pharmacological strategies have emerged, based on the latest generation of analgesics, which have revolutionized intervention strategies for patients. As a consequence of these advances, the field of nursing has also updated its protocols and procedures, adjusting to the new times and equipment. However, health care professionals find it difficult to keep up to date on these aspects due to the lack of educational programs on this subject, focused on their specific competencies.
For this reason, TECH has designed this Hybrid professional master’s degreee in Pain Management for Nursing. Through this program, graduates will have access to all the most modern knowledge in this field with an academic modality divided into two stages. First, dedicated to the theoretical study of the field of care in question, will take place on a 100% online and interactive platform. In it, the contents will be free from the very beginning, facilitating self-management of learning. In addition, to reinforce knowledge more effectively, you will use a variety of multimedia resources such as interactive summaries, videos and infographics. Likewise, Relearrning, a methodology of great didactic value, will contribute to assimilate new skills in a fast and flexible way.
In the second half, students will develop a first level clinical practice, in a hospital center equipped with the best technologies and healthcare resources. In this way, the nurse will be able to learn first-hand all its applications and develop the procedures specific to his or her area of work to contribute to the evaluation and recovery of patients. Throughout this intensive 3-week on-site stay, you will discuss management strategies with leading experts. At the same time, an assistant tutor will supervise your work and assign tasks to increase your progress.
With this program, you will have total comfort to self-manage the study of its theoretical contents through 1,500 hours of learning"
This Hybrid professional master’s degree in Pain Management for Nursing contains the most complete and up-to-date Scientific program on the market. Its most notable features are:
- Development of more than 100 clinical cases presented by nursing experts in chronic pain management.
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice.
- Comprehensive systematized action plans for the main pathologies Presentation of practical workshops on diagnostic and therapeutic techniques
- Practical clinical guides on approaching different pathologies
- All of this will be complemented by theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments.
- Content that is accessible from any fixed or portable device with an Internet connection.
- Furthermore, you will be able to carry out a clinical internship in one of the best hospital centers
Destinarás 3 semanas al desarrollo de habilidades prácticas enfermeras, relacionadas con el Abordaje del Dolor, por medio de este completísimo Hybrid professional master’s degree”
In this Hybrid professional master’s degree, with a vocational nature and blended learning modality, the program is aimed at updating nursing professionals who require a high level of qualification. The content is based on the latest scientific evidence and is organized in a didactic way to integrate theoretical knowledge into nursing practice.
The theoretical-practical elements allow professionals to update their knowledge and help them to make the right decisions in patient care.Thanks to the multimedia content, developed with the latest educational technology, nursing professionals will benefit from situated and contextual learning, i.e., a simulated environment that will provide immersive learning programmed to train in real situations. This program is designed around Problem-Based Learning, whereby the physician must try to solve the different professional practice situations that arise during the course. For this purpose, the students will be assisted by an innovative interactive video system created by renowned and experienced experts.
This Hybrid professional master’s degree will update you on the technical aspects to be taken into account to objectively assess the communication and behavior of the patient who claims to suffer acute pain"

Master the most modern procedures on epidural infiltrations and how to assist the physician in their development from your role as a nurse"
Teaching Planning
The syllabus of this program provides an exhaustive up-to-date on the most advanced procedures and protocols for the Nursing staff to deal with pain. Its academic modules cover topics such as the most modern scales for differentiating pain and how health care professionals can contribute to its evaluation. The agenda also examines the techniques that nurses can apply to help physicians intervene in this type of problem. To master all these subjects, TECH provides theoretical learning guides accompanied by excellent multimedia materials such as videos, infographics and interactive summaries.

In the first stage of this Hybrid professional master’s degree, you will be able to access all the contents, from the first day, on a 100% online and interactive platform"
Module 1. General Pain Concepts for Nursing
1.1. Concept of Pain and Its Evolution in Time
1.2. Etiology of Pain
1.2.1. Nociceptive Pain
1.2.2. Neuropathic Pain
1.2.3. Psychogenic Pain
1.3. Classification
1.3.1. According to Seasonality
1.3.2. According to Intensity
1.3.3. According to Location: Somatic and Visceral
1.3.4. According to Its Course
1.4. Neuroanatomy and Neurobiology of Pain
1.5. Pathophysiology of Pain
1.5.1. Neurophysiological Processes Involved in Pain
1.6. Complementary Tests for the Diagnosis of Pain
1.6.1. Nerve Conduction Velocity Study
1.6.1.1. Electromyography
1.6.1.2. Thermography
1.6.1.3. Brain Evoked Potentials
1.6.1.4. Functional MRI
1.6.1.5. Somatosensory Quantitative Thermal Test
1.7. Clinical History and Physical Examination of the Patient with Pain
1.7.1. Medical History
1.7.2. Pain Intensity Rating Scales
1.8. Interventional Pain Techniques
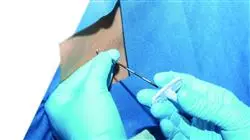
1.8.1. Epidural Infiltrations
1.8.2. Intradural Administration of Drugs
1.8.2.1. Radiofrequency
1.8.2.2. Neurolytic Blocks
1.8.2.3. Neurostimulation
1.9. Use of Analgesics and Pharmacology
1.9.1. Basic Principles
1.9.2. OMS Ladder and Analgesic Elevator
1.9.3. Drugs: Non-Opioids, Opioids and Adjuvants
1.10. Future of Pain Assessment and Treatment
1.10.1. Development of New Analgesic Drugs
1.10.2. Development of Alternative Analgesic Drug Delivery Systems for Infusion Pumps
1.10.3. Gene Therapy for the Treatment of Pain
Module 2. Acute and Postoperative Pain for Nursing
2.1. Types of Acute Pain
2.2. Units of Acute Pain
2.2.1. Infrastructure
2.2.2. Care Models
2.3. Nursing Intervention in Acute Pain
2.3.1. Assessment of Acute Pain
2.3.2. Pharmacological Interventions for Acute Pain
2.3.3. Non-Pharmacological Interventions for Acute Pain
2.4. Acute Postoperative Pain
2.4.1. Definition
2.4.2. Incidence and Prevalence of Acute Postoperative Pain
2.4.3. Evaluation of Acute Postoperative Pain
2.5. Treatment of Postoperative Pain
2.5.1. Prevention of Postoperative Pain
2.5.2. Types of Treatment for Postoperative Pain
2.5.3. Medical Treatment
2.5.4. Non-Pharmacological Treatment
2.6. Safety of the Surgical Patient
2.7. Postoperative Morbidity
2.7.1. Causes: Pain and Interventionism
2.7.2. Solutions
2.8. Surgical Nursing and Pain
2.8.1. Topic Update
2.8.2. Protocols and Interventions Evaluated
2.9. Perioperative Nursing in Anxiety and Pain
2.10. Latest Trends and Improvements in Acute Pain Management for Nursing
2.10.1. Innovation in Acute Pain
2.10.2. Innovation in Postoperative Pain
Module 3. Chronic Oncologic Pain for Nursing
3.1. The Oncology Patient and Pain
3.1.1. Pathophysiology
3.1.2. Main Causes of Pain in the Oncology Patient
3.2. Types of Pain
3.2.1. Signs and Symptoms
3.2.2. According to Evolution Time
3.2.3. According to Its Pathophysiological Mechanism
3.2.4. According to Etiology
3.3. Nursing Assessment and Evolution of Pain
3.3.1. Pain History
3.3.2. Clinical and Psychological Examination
3.3.3. Pain Measurement Scales and Questionnaires
3.3.4. Diagnostic Tests
3.4. Procedures and Treatments of the Cancer Patient Causing Pain for Nursing
3.4.1. Chemotherapy
3.4.2. Biological Techniques and Immunotherapy
3.4.3. Hormone Therapy
3.4.4. Radiotherapy
3.4.5. Surgery
3.5. Cancer-Related Fatigue
3.5.1. Etiology
3.5.2. Risk Factors
3.5.3. Signs and Symptoms
3.6. Medical Treatment
3.6.1. Analgesic Scale
3.6.2. Adjuvant Drugs
3.6.3. Bisphosphonates
3.6.4. Side Effects
3.6.5. Route of Administration
3.6.6. Palliative Care
3.7. Invasive or Special Analgesic Techniques
3.7.1. Nerve Blocker
3.7.2. Neurostimulation
3.7.3. Surgical intervention
3.7.4. Radiotherapy
3.7.5. Palliative Chemotherapy
3.7.6. Physical Therapy
3.7.7. Psychological Therapy
3.8. Integrative Medicine for Nursing
3.8.1. Massage, Acupuncture
3.8.2. Yoga, Meditation
3.9. Identifying Oncologic Emergencies Through Pain
3.9.1. Signs and Symptoms Related to Oncologic Emergencies
3.10. Nursing Care Plans
3.10.1. Nursing Assessment
3.10.2. Nursing Diagnosis
3.10.3. NOC/NIC
Module 4. Chronic Non-Oncologic Pain for Nursing
4.1. Introduction
4.1.1. Definition of Chronic Pain
4.1.2. Description of Non-Oncologic Chronic Pain
4.2. Epidemiology of Non-Oncologic Chronic Pain
4.2.1. How Many Spaniards Suffer from Pain?
4.2.1.1. Who Suffers the Most Pain?
4.2.1.2. Most Frequent Pain Among Spaniards
4.2.1.3. Consequences of Pain
4.2.1.4. Prevalence of Chronic Pain in Spain
4.3. Etiopathogenesis
4.3.1. Nociceptive Pain
4.3.2. Somatic Pain
4.3.3. Visceral Pain
4.3.4. Neuropathic Pain
4.4. Neuropathic Pain
4.4.1. Trigeminal Neuralgia
4.4.2. Postherpetic Neuralgia
4.4.3. Diabetic Neuralgia
4.4.4. Ilioinguinal Neuralgia
4.5. Phantom Limb Pain
4.5.1. Definition
4.5.2. Clinical Manifestations
4.5.3. Etiology
4.5.4. Recommendations in Nursing
4.6. Complex Regional Pain Syndrome
4.6.1. Definition
4.6.2. Prevalence
4.6.3. Causes and Classifications
4.6.4. Triggering Factors
4.6.5. Treatment
4.6.6. Recommendations in Nursing
4.7. Central Pain syndrome
4.7.1. Definition
4.7.2. Etiology
4.7.3. Epidemiology
4.7.4. Clinical Manifestations
4.7.5. Treatment
4.7.6. Recommendations in Nursing
4.8. Headaches
4.8.1. Types
4.8.2. Diagnosis
4.8.3. Secondary Headaches
4.8.4. Recommendations in Nursing
4.9. Other Syndromes
4.9.1. Chronic Pancreatitis
4.9.2. Coccygodynia
4.9.3. Prostatodynia
4.9.4. Vulvodynia
4.10. Pain Unit
4.10.1. Nursing Skills
4.10.2. Organization of the Pain Unit
4.10.3. Nursing Team Roles
4.10.4. Nursing Intervention in Certain Techniques
Module 5. Pain in Children for Nursing
5.1. Basic Concepts of Pain
5.1.1. Concept
5.1.2. Epidemiology
5.1.3. Neurophysiology of Pain
5.1.4. Pain Neuropathology
5.1.5. Influencing Factors
5.1.6. False beliefs
5.2. Pain Classification Forms of Expression of Pain According to the Child's Developmental Stages
5.2.1. Types of Pain: Pathophysiologic, Duration, Etiologic, Anatomic
5.2.2. Pain According to the Evolutionary Stages of the Child
5.2.3. Consequences of Pain in Children
5.3. Pain Assessment I
5.3.1. Behavioral Methods
5.3.2. Physiological Methods
5.4. Pain Assessment II
5.4.1. Self-Assessment Methods: Projective, Structured Interviews, and Scales
5.5. Pharmacological Treatment of Pain in Children
5.6. Non-pharmacological Treatment of Pain in Children
5.7. Pain in Neonates
5.8. Pain in Children with Cancer
5.9. Pain in Hospitalized Children Related to Techniques
5.10. Pain in Children Undergoing Intensive Care
Module 6. Musculoskeletal Pain for Nursing
6.1. Introduction and Concepts
6.1.1. Concept of Musculoskeletal Pain
6.1.2. Epidemiology and Impact of the Processes
6.1.3. Pathophysiology
6.1.4. Clinical Characteristics
6.1.5. Classification
6.2. Nurse Assessment of Pain
6.2.1. Verbal Assessment Methods
6.2.2. Behavioral Assessments
6.2.3. Physiological Measurements
6.3. Inflammatory Pain
6.3.1. Features
6.3.2. Epidemiology
6.3.3. Inflammatory Arthropathies
6.4. Mechanical Pain
6.4.1. Features
6.4.2. Epidemiology
6.4.3. Degenerative Arthropathies
6.4.4. Soft Tissue Alteration
6.5. Musculoskeletal Pain in Bone Diseases
6.5.1. Characteristics of Bone Diseases
6.5.2. Epidemiology
6.5.3. Pain in Osteoporosis
6.5.4. Pain in Paget’s Disease
6.5.5. Osteoarticular Pain
6.6. Musculoskeletal Pain Due to Metabolic and Endocrine Disorders
6.6.1. Definition of Metabolic and Endocrine Disorders
6.6.2. Epidemiology
6.6.3. Classification
6.6.4. Pain Due to Metabolic and Endocrine Disorders
6.7. Muscular Pain
6.7.1. Introduction
6.7.1. Features
6.7.2. Epidemiology
6.7.3. Myofascial Pain
6.7.4. Fibromyalgia
6.8. Musculoskeletal Pain in Connective Tissue Diseases
6.8.1. Definition in Connective Tissue Diseases
6.8.2. Epidemiology
6.8.3. Classification
6.8.4. Pain in Connective Tissue Diseases
6.9. Treatment of Musculoskeletal Pain
6.9.1. Oral Treatment
6.9.2. Topical treatment
6.9.3. Nerve Blocks and Infiltration Techniques
6.9.4. Radiofrequency Techniques
6.9.5. Neuromodulation Techniques
6.10. Roles of the Nurse in the Management of the Patient with Musculoskeletal Pain
Module 7. Psychological Approach to Pain for Nursing
7.1. Communication with the Patient (Nursing Perspective)
7.1.1. Importance of Good Communication with the Patient
7.1.2. Types of Communication
7.1.3. Improving Communication
7.2. Psychological Aspects of Pain, Psychological Problems
7.2.1. Anxiety
7.2.2. Depression
7.2.3. Insomnia
7.2.4. Low self-esteem
7.3. Psychological Aspects of Pain, Personal Relationship Problems
7.3.1. With Family
7.3.2. With the Partner
7.3.3. Sexuality
7.3.4. Voluntary Isolation
7.4. Psychological Aspects of Pain
7.4.1. Quality of Life: Decrease in Physical Activity, Lack of Independence, Decrease in Leisure & Entertainment
7.4.2. Economic Problems: Sick Leave, Health Care Costs, Disability, etc
7.5. Coping with Pain: Relaxation
7.5.1. Types of Relaxation
7.5.2. Relaxation Training
7.6. Coping with Pain: Cognitive Behavioral Treatment I
7.7. Coping with Pain: Cognitive Behavioral Treatment II
7.8. Coping with Pain: Clinical Hypnosis
7.9. Coping with Pain I
7.9.1. Biofeedback
7.9.2. Acceptance and Commitment Therapy
7.9.3. Emotional Writing
7.10. Coping with Pain II
7.10.1. Mindfulness
7.10.2. New Technologies
Module 8. Pain Management through Rehabilitation and Physical Activity for Nursing
8.1. Introduction to Pain
8.1.1. Introduction to Pain
8.1.2. Definition of Pain
8.1.3. Pain Models
8.1.4. Clinical Implications in Each Model
8.2. Introduction to Clinical Reasoning
8.2.1. Definition of Clinical Reasoning
8.2.2. Clinical Reasoning Models
8.2.3. Hypothesis Categories
8.3. Pathobiological Mechanisms of Pain
8.3.1. Mature Organism Model
8.3.2. Input: Nociceptive Pain
8.3.3. Inflammatory Pain
8.3.4. Peripheral Neuropathic Pain
8.3.5. Processing: Maladaptive Pain
8.3.6. Output: Organism Response
8.4. Nociceptive Pain
8.4.1. Clinical Characteristics
8.4.2. Characteristics of the Tissues
8.4.3. Healing Ability
8.4.4. Basic Treatment Principles
8.4.5. Clinical Implications
8.5. Neuropathic Pain
8.5.1. Clinical Features: Negative Signs vs. Positive Symptoms
8.5.2. Physiology of Nerve Injury
8.5.2.1. Prognosis
8.5.2.2. Treatment Principles
8.6. Complex Chronic Pain
8.6.1. Clinical Characteristics
8.6.2. Pain Identifiers
8.6.3. Theories of Complex Chronic Pain
8.6.4. Specificity vs Peripheral Pattern
8.6.5. Neuromatrix Theory
8.6.6. Relevance Theory
8.6.7. Dynamic Connectome Theory
8.7. Risk Factors for Chronicity
8.7.1. Psychosocial Factors
8.7.2. Social and Cultural Factors
8.8. Fear of Movement
8.8.1. Fear-Avoidance Model
8.9. Treatment
8.9.1. Manual Therapy
8.9.2. Educational
8.9.3. Exercise
8.10. Treatment of Complex Chronic Pain
8.10.1. Pain Education
8.10.2. Gradual Exposure to Movement
8.10.3. Behavioral Changes
Module 9. Nurse Assessment and Intervention in Pain
9.1. Standardized Nursing Assessment
9.1.1. Assessment as a Phase of Nursing Methodology
9.1.2. The Nursing Assessment Process
9.1.3. Assessment According to Functional Patterns of Health
9.1.4. Assessment According to Basic Human Needs
9.2. The Importance of Pain Assessment: The Fifth Sense
9.2.1. Pain as a Multidimensional Experience
9.2.2. Nursing Knowledge and Beliefs About Pain
9.2.3. Barriers to Good Pain Management
9.3. Localized Pain Assessment Protocol
9.3.1. Medical History
9.3.2. Medical and Surgical Background
9.3.3. Family and Social Background
9.3.4. Psychiatric Background
9.3.5. History of Pain
9.3.6. Physical Examination
9.3.7. Explore Knowledge and Beliefs about Pain
9.3.8. Pain Reassessment
9.4. Pain Assessment Scales I: One-Dimensional and Multidimensional Scales
9.4.1. One-dimensional Scales
9.4.2. Multidimensional Scales
9.5. Pain Assessment Scales II: Special Situations
9.5.1. For Patients Unable to Speak
9.5.2. For Patients with Dementia
9.6. Comprehensive Assessment of Human Responses to Pain
9.6.1. Breathing
9.6.2. Feeding
9.6.3. Elimination
9.6.4. Mobilization
9.6.5. Rest and Sleep
9.6.6. Getting Dressed and Undressed
9.6.7. Temperature
9.6.8. Hygiene and Skin Condition
9.6.9. Security/Safety
9.6.10. Communication/Relationship
9.6.11. Beliefs/Religion
9.6.12. Learning
9.6.13. Self-realization
9.6.14. Leisure
9.7. Nursing Care Plan for Pain I
9.8. Nursing Care Plan for Pain II
9.9. Non-Pharmacological Management of Pain
9.9.1. Physical Measurements
9.9.2. Environmental Measurements
9.9.3. Measures for the Promotion of Psychological Comfort
9.9.4. Measures to Aid Coping
9.10. Health Education for Patients and Their Family
9.10.1. Individual Therapy
9.10.2. Group
9.10.3. Pharmacy
Module 10. Epidemiology and Public Health for Nursing
10.1. The Concept of Public Health
10.1.1. Definition of Public Health
10.1.2. Acute Pain and Public Health
10.1.3. Chronic Pain and Public Health
10.1.4. Oncologic Pain and Public Health
10.2. Health Politics Regarding Pain
10.2.1. Plan for the Improvement of Pain Care in the Spanish National Health System
10.3. Demographics of Pain
10.4. Gender and Pain
10.4.1. Women and Chronic Pain
10.4.2. Social Impact of Pain in Women
10.4.3. Women and Chronic Disease
10.5. Social and Labor Impact of Pain in Spain
10.5.1. Studies of the Social and Occupational Impact of Pain in Spain
10.5.2. Disability and Pain
10.6. Epidemiology of Cancer Pain
10.6.1. Current Epidemiology of Oncological Pain
10.6.2. Social and Economic Consequences
10.7. Sexuality in People with Chronic Pain
10.7.1. Current Epidemiology of Chronic Pain
10.7.2. Social and Economic Consequences
10.8. Epidemiology of Acute Pain
10.8.1. Current Epidemiology of Acute Pain
10.8.2. Social and Economic Consequences
10.9. Bioethics of Pain
10.9.1. Bioethics General concepts
10.9.2. Bioethics and Chronic Pain
10.9.3. Bioethical Implications in Pain Management
10.10. Health promotion
10.10.1. Community Health Promotion
10.10.2. Hospital Measures to Promote Health in Chronic Patients
10.10.3. Associative Movement and Health Promotion

Relearning, a didactic method created and applied by TECH , it will allow you to consolidate theoretical concepts in a faster and more flexible way"
Hybrid Professional Master's Degree in Pain Management for Nursing
If you are a nurse and want to become an expert in pain management, the Hybrid Professional Master's Degree in Pain Management for Nursing from TECH Global University is your gateway to a more rewarding and opportunity-filled career. We are committed to providing high-quality graduate programs that drive professional growth. Our Master's degree is designed to provide you with comprehensive learning in pain management, from the most current techniques to the associated psychological and emotional aspects. During 1 year, you will combine the convenience of studying from home the theoretical part combined with practical classes in a face-to-face environment. Our team of highly trained faculty with extensive experience in the field of pain will guide you through a rigorous and up-to-date curriculum.
Master Advanced Pain Management Techniques in Nursing.
Do you know why TECH is considered one of the best universities in the world? Because we have a catalog of more than ten thousand academic programs, presence in multiple countries, innovative methodologies, unique academic technology and a highly qualified teaching team. The Hybrid Professional Master's Degree in Pain Management for Nurses will allow you to acquire specialized knowledge in areas such as pain pathophysiology, assessment and diagnostic techniques, pharmacology, non-pharmacological therapies and palliative care. You will also develop practical skills through clinical simulations and supervised internships. Upon completion of the Master's degree, you will be prepared to assume a leadership role in pain management, applying advanced techniques and providing quality patient care. Enroll now and take a step forward in your career!







