University certificate
Accreditation/Membership
.png)
The world's largest faculty of medicine”
Introduction to the Program
With this 100% online Master's Degree, you will take a comprehensive approach to Pediatric Emergency Medicine and significantly optimize the quality of life of your patients”

Pediatric Emergencies have undergone significant development and professionalization in recent years, requiring physicians to stay updated in order to provide comprehensive care based on the latest scientific evidence. To achieve this, continuous knowledge updates are essential, enabling physicians to act effectively in Pediatric Emergency Services.
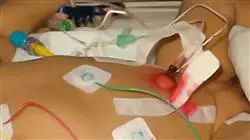
Updating knowledge in this field is necessary not only to recognize and resolve emergencies immediately, but also to appropriately guide the management of conditions that require follow-up. The training of physicians in Pediatric Emergencies should include learning and updating essential diagnostic and therapeutic techniques, such as airway management, access to peripheral and central lines, and immobilization of patients with trauma or burns. Additionally, it is key to understand the organization of emergency services, ensuring proper distribution of personnel and resources.
In this context, TECH Master's Degree in Pediatric Emergencies offers medical professionals updated knowledge on the main Pediatric Emergencies, providing tools for managing critically ill patients and using the most advanced diagnostic and treatment techniques. Moreover, its 100% online modality offers flexible training adapted to the needs of each student.
Furthermore, professionals will have exclusive access to Masterclasses delivered by renowned International Guest Directors. These sessions will allow them to strengthen their skills and knowledge in an increasingly in-demand field, ensuring more effective and safer patient care.
Renowned International Guest Directors will deliver intensive Masterclasses on the latest innovations in Pediatric Emergency Medicine management”
This Master's Degree in Pediatric Emergencies contains the most complete and up-to-date university program on the market. Its most notable features are:
- The development of practical case studies presented by experts in Medicine
- The graphic, schematic, and practical contents with which they are created, provide scientific and practical information on the disciplines that are essential for professional practice
- Practical exercises where the self-assessment process can be carried out to improve learning
- Special emphasis on innovative methodologies in the management of audiovisual industries
- Theoretical lessons, questions to the expert, debate forums on controversial topics, and individual reflection assignments
- Content that is accessible from any fixed or portable device with an Internet connection
You will master the most modern advanced cardiopulmonary resuscitation and pediatric life support techniques, ensuring an optimal response in critical situations”
The teaching staff includes professionals belonging to the field of medicine, who contribute their work experience to this program, as well as renowned specialists from reference societies and prestigious universities.
The multimedia content, developed with the latest educational technology, will provide the professional with situated and contextual learning, i.e., a simulated environment that will provide an immersive educational experience designed to prepare students for real-life situations.
This program is designed around Problem-Based Learning, whereby students must try to solve the different professional practice situations that arise during the academic year. For this purpose, professionals will be assisted by an innovative interactive video system created by renowned and experienced experts.
Thanks to TECH Relearning you will be able to assimilate the essential concepts in a fast, natural and accurate way"
You will develop advanced skills in the evaluation and management of critically ill pediatric patients, applying updated emergency care protocols"
Syllabus
This Master's Degree program offers a comprehensive curriculum designed for professionals to approach Pediatric Emergency Medicine based on the latest evidence.
Through structured modules, graduates will delve into the most effective life support and cardiopulmonary resuscitation techniques to stabilize patients. In this way, healthcare providers will be trained to interpret diagnostic tests in real time, administer appropriate treatments based on the pathology, and coordinate with multidisciplinary teams to optimize patient outcomes.

Master the latest techniques in Pediatric Emergency Ophthalmology Protocols and become a well-rounded professional in the healthcare field”
Module 1. Healthcare Organization in Response to Common Pediatric Emergencies
1.1. Equipment in the Pediatric Emergency Department (PED)
1.1.1. Differential Characteristics of PEDs
1.1.2. Infrastructure, Staffing
1.1.3. Material
1.2. Triage in Pediatrics
1.2.1. Definition
1.2.2. Classification Systems
1.3. Transport of Critical Pediatric Patient. In-hospital Transfer, Out-of-Hospital Transfer and ISOBAR
1.4. Neonatal and Pediatric Transportation
Module 2. Advanced Pediatric and Neonatal Cardiovascular Support
2.1. Apparently Lethal Syndromes
2.1.1. Sudden Infant Death
2.1.2. Treatment
2.1.3. Home Monitoring
2.2. Recognition and Management of Critically Ill Children
2.2.1. Epidemiology, Etiology and Prevention of CRP in Childhood
2.2.2. Pediatric Assessment Triangle (PAT) and its Utility
2.2.3. Pediatric ABCDE Assessment
2.3. Basic Pediatric Cardiopulmonary Resuscitation
2.4. Advanced Pediatric Cardiopulmonary Resuscitation. Advanced Airway Management
2.5. Basic Concepts of Mechanical Ventilation
2.6. Infusion Routes and Drugs
2.7. Pediatric Advanced Life Support (PALS) Algorithms and Arrhythmia Treatment
2.8. Neonatal Resuscitation
2.9. Stabilization, Post-Resuscitation and Neonatal Transportation
Module 3. Invasive Techniques in Common Critically Ill Pediatric Patients
3.1. Peripheral and Central Vein Access
3.1.1. Peripheral Route
3.1.2. Central Route
3.2. Intraosseous Puncture
3.3. Capnography. Pulse Oximetry
3.4. Oxygen Therapy
3.5. Analgesia and Sedation
3.5.1. Pain Management
3.5.2. Procedure
3.5.3. Reference Drugs in Analgesia and Sedation
3.6. Protocol for Child Death
3.7. Rapid Sequence Intubation
Module 4. Cardiovascular Emergencies
4.1. Arrhythmias and Syncope
4.1.1. Bradyarrhythmias Diagnosis and Treatment
4.1.2. Tachyarrhythmias. Diagnosis and Treatment
4.2. Congenital Heart Disease
4.2.1. Cyanotic Congenital Heart Disease
4.2.2. Non-Cyanotic Congenital Heart Disease
4.2.3. Diagnostic Approach
4.2.4. Treatment
4.3. Hypertensive Crisis
4.3.1. Diagnostic Guidance for Hypertension in Children and Adolescents
4.3.2. Therapeutic Guidance for Hypertension in Children and Adolescents
4.4. Heart Failure
4.4.1. Etiology
4.4.2. Diagnosis
4.4.3. Treatment. Mechanical Ventricular Assistance Techniques. Extracorporeal Membrane Oxygenation (ECMO)
4.5. Quick Reading of an ECG
4.6. Management of Tachyarrhythmias and Bradyarrhythmias: Electrical Cardioversion and Transcutaneous Pacing
4.7. Management of Defibrillable Arrhythmias: Defibrillation
Module 5. Respiratory Emergencies
5.1. Respiratory Pathology of Newborns
5.1.1. Incomplete Pulmonary Fluid Reabsorption Syndrome
5.1.2. Meconium Aspiration Syndrome
5.1.3. Hyaline Membrane Disease
5.1.4. Pneumothorax
5.1.5. Pneumonia
5.1.6. Apnea in Newborns
5.2. Airway Diseases
5.2.1. Acute Pharyngotonsillitis
5.2.2. Laryngitis or Croup
5.2.3. Spasmodic Croup
5.2.4. Otitis
5.2.5. Sinusitis
5.3. Community-Acquired Pneumonia (CAP)
5.3.1. Diagnosis
5.3.2. Hospital Admission Criteria
5.3.3. Latest Advances in Treatment
5.4. Managing the Coughing Child. Chronic Cough
5.4.1. Etiology
5.4.1.1. Persistent Bacterial Bronchitis
5.4.1.2. Asthma
5.4.1.3. Gastroesophageal Reflux, etc.
5.4.2. Treatment
5.5. Asthma Care in Children
5.5.1. Clinical Diagnosis. Functional Diagnosis
5.5.2. Pharmacological Treatment. Non-Pharmacological Treatment
5.5.3. Health Education
5.6. Inhalation Techniques. Oxygen Therapy
5.7. Thoracentesis and Chest Tube Placement
5.8. Forced Spirometry. Bronchodynamic Tests. PEF (Peak Expiratory Flow)
Module 6. Pediatric Trauma and Osteoarticular Injuries
6.1. Initial Pediatric Trauma Care
6.1.1. Types and Patterns of Injury in Pediatrics
6.1.2. Primary and Secondary Assessment
6.1.3. Spinal Cord Injuries
6.2. Head Trauma in Children
6.3. Lower Extremity Trauma
6.4. Upper Limb Trauma
6.5. Thoracic Trauma. Rib Fractures and Contusions
6.6. Limping
6.6.1. Types of Lameness
6.6.2. Treatment
6.6.3. Referral Criteria
6.7. Classification of Pediatric Fractures
6.8. Mobilization and Immobilization Workshop
6.9. Active Mobilization Stimulation
6.10. Hyperpronation
6.11. Supination-Flexion
6.12. Radial Head Subluxation
Module 7. Unintentional Injuries. Childhood Accidents
7.1. Wounds
7.2. Burns
7.3. Drowning
7.4. Stings and Bites
7.5. Drug and Non-drug Intoxications
7.6. Anaphylaxis
7.6.1. Classification of Severity
7.6.2. Diagnostic Procedures
7.6.3. Treatment and Discharge Recommendations
7.7. Extraction of Foreign Body from the Ear
7.8. Extraction of Foreign Bodies from the Nose
7.9. Freeing of Trapped Penis or Scrotum
7.10. Incarcerated Inguinal Hernia Reduction
7.11. Reduction of Paraphimosis
Module 8. Neurological Emergencies
8.1. Acute Ataxia
8.2. Alterations of Consciousness
8.3. Acute Headache
8.3.1. Migraine
8.3.2. Tension Headache
8.3.3. Periodic Syndromes of Childhood
8.4. Epilepsies and Non-Epileptic Seizure Disorders in Childhood
8.4.1. Epileptic Syndromes in Childhood and Adolescence
8.4.2. General Treatment of Epilepsies
8.5. Bacterial and Viral Meningitis
8.6. Febrile Seizures
8.7. Puncture of the Ventriculoperitoneal Shunt Reservoir
8.8. Lumbar Puncture
Module 9. Digestive Emergencies
9.1. The Infant with Food Refusal
9.2. Acute Abdominal Pain
9.3. Gastrointestinal Disorders
9.4. Acute Dehydration
9.4.1. Isonatremic Dehydration
9.4.2. Hyponatremic Dehydration
9.4.3. Hypernatremic Dehydration
9.5. Acid-Base Balance Disorders
9.5.1. Metabolic Acidosis. Respiratory Acidosis
9.5.2. Metabolic Alkalosis. Respiratory Alkalosis
9.6. Celiac Disease
9.6.1. Diagnostic Algorithm
9.6.2. Treatment
9.7. Gastroesophageal Reflux (RGE)
9.8. Constipation
9.9. Hepatitis
9.9.1. HAV, HBV, HCV, HDV, HEV
9.9.2. Autoimmune Hepatitis
9.10. Gastrointestinal Bleeding
9.11. Jaundice
Module 10. Endocrine and Metabolic Emergencies
10.1. Emergencies in the Diabetic Patient
10.2. Hydroelectrolytic Alterations
10.3. Adrenal Insufficiency
Module 11. Infectious Emergencies
11.1. Exanthematous Diseases
11.2. Whooping Cough and Pertussis-Like Syndrome
11.2.1. Pharmacological Treatment
11.2.2. Control Measures
11.3. Febrile Syndrome without Focus
11.4. Sepsis. Septic Shock
11.5. Osteoarticular Infections
11.6. Fever and Neutropenia
Module 12. Ophthalmic and Otolaryngologic Emergencies
12.1. Conjunctivitis and Blepharitis. Red Eye
12.1.1. Most Frequent Infectious Pathology
12.1.2. Non-Infectious Pathology
12.1.3. Pediatric Ophthalmic Emergency Protocol
12.2. Eyelids and Lacrimal System
12.2.1. Palpebral Alterations and Malformations
12.2.2. Inflammatory Pathology
12.2.3. Cysts and Tumors
12.2.4. Lacrimal Pathology in Children
12.2.5. Palpebral Trauma in Childhood
12.3. Acute Pharyngotonsillitis. Acute Otitis Media Sinusitis
12.4. Extraction of Foreign Bodies from the Eye
12.5. Ophthalmologic Examination with Fluorescein
12.6. Eversion of the Upper Eyelid
Module 13. Pediatric Dermatological Emergencies
13.1. Bacterial Infections in Pediatrics
13.1.1. Contagious Impetigo
13.1.2. Folliculitis, Furunculosis and Carbuncles
13.1.3. Perianal Streptococcal Dermatitis
13.2. Viral Infections in Pediatrics
13.2.1. Human Papiloma Virus
13.2.2. Molluscum Contagiosum
13.2.3. Herpes Simplex
13.2.4. Shingles
13.3. Mycotic Infections in Pediatric Dermatology
13.3.1. Tinea
13.3.2. Candidiasis
13.3.3. Pityriasis Versicolor
13.4. Infestations in Pediatric Dermatology
13.4.1. Pediculosis
13.4.2. Scabies
13.5. Eczema. Atopic Dermatitis
Module 14. Renal and Urological Emergencies
14.1. Urinary Infections
14.1.1. Diagnostic Criteria
14.1.2. Referral Indications
14.2. Hematuria
14.3. Renal Lithiasis and Renal Colic
14.4. Acute Scrotum
14.4.1. Frequency in the Pediatric Age Group
14.5. Suprapubic Puncture
14.6. Bladder Catheterization
14.7. Reduction of Paraphimosis
Module 15. Special Situations in Pediatric Emergencies
15.1. Children with Special Needs
15.1.1. Tracheostomy and Home Mechanical Ventilation
15.1.2. Gastrostomies and Feeding Tubes
15.1.3. Peritoneal Ventriculo-Peritoneal Shunt Valves
15.1.4. Central Catheters and Prosthetic Vascular Accesses
15.2. Medication in Pediatrics
15.3. Psychiatry in the Emergency Department
15.3.1. Assessment and Initial Treatment
15.3.2. Psychomotor Agitation and Violence
15.3.3. Suicidal Behavior
15.3.4. Psychotic Disorders
15.4. Child Abuse
15.4.1. Attitude in the Emergency Room
15.4.2. Assistance in the Case of Abuse
15.5. Techniques and Procedures. Mechanical Restraint of the Agitated or Aggressive Child
Module 16. Current Status of Coronavirus Infections
16.1. Discovery and Evolution of Coronaviruses
16.1.1. Discovery of Coronaviruses
16.1.2. Global Trends in Coronavirus Infections
16.2. Main Microbiological Characteristics and Members of the Coronavirus Family
16.2.1. General Microbiological Characteristics of Coronaviruses
16.2.2. Viral Genome
16.2.3. Principal Virulence Factors
16.3. Epidemiological Changes in Coronavirus Infections from Discovery to the Present
16.3.1. Morbidity and Mortality of Coronavirus Infections from their Emergence to the Present
16.4. The Immune System and Coronavirus Infections
16.4.1. Immunological Mechanisms Involved in the Immune Response to Coronaviruses
16.4.2. Cytokine Storm in Coronavirus Infections and Immunopathology
16.4.3. Modulation of the Immune System in Coronavirus Infections
16.5. Pathogenesis and Pathophysiology of Coronavirus Infections
16.5.1. Pathophysiological and Pathogenic Alterations in Coronavirus Infections
16.5.2. Clinical Implications of the Main Pathophysiological Alterations
16.6. Risk Groups and Transmission Mechanisms of Coronaviruses
16.6.1. Main Sociodemographic and Epidemiological Characteristics of Risk Groups Affected by Coronavirus
16.6.2. Coronavirus Mechanisms of Transmission
16.7. Natural History of Coronavirus Infections
16.7.1. Stages of Coronavirus Infection
16.8. Updated Microbiological Diagnosis of Coronavirus Infections
16.8.1. Sample Collection and Shipment
16.8.2. PCR and Sequencing
16.8.3. Serology Testing
16.8.4. Virus Isolation
16.9. Current Biosafety Measures in Microbiology Laboratories for Coronavirus Sample Handling
16.9.1. Biosafety Measures for Coronavirus Sample Handling
16.10. Up-to-Date Management of Coronavirus Infections
16.10.1. Prevention Measures
16.10.2. Symptomatic Treatment
16.10.3. Antiviral and Antimicrobial Treatment in Coronavirus Infections
16.10.4. Treatment of Severe Clinical Forms
16.11. Future Challenges in Prevention, Diagnosis, and Therapy of Coronavirus Infections
16.11.1. Global Challenges for the Development of Prevention, Diagnostic, and Treatment Strategies for Coronavirus Infections

Enjoy an intensive 3-week stay in a prestigious center and update yourself on the latest procedures to grow professionally”
Master's Degree in Pediatric Emergencies
With the goal of providing the best education available in the medical field, TECH Global University has designed the most sophisticated and specialized Master's Degree in Pediatric Emergency Medicine on the educational market. This comprehensive program offers you the opportunity to update your knowledge and become a professional with the highest quality standards. Upon completing the degree, you will have the necessary skills to apply diagnostic and therapeutic techniques to pediatric patients with urgent pathologies, aiming to provide emergency care that improves the child's prognosis and supports the care of their family.
Postgraduate in treatment of pediatric patients in emergency situations
Our postgraduate program gives you the opportunity to learn the latest advances related to diagnostic and therapeutic procedures for various infections caused by hepatitis viruses: HAV, HBV, HCV, HDV, HEV. Additionally, it qualifies you to develop and apply sequences in different workshops for mobilizing and immobilizing traumatic patients, such as functional bandaging, casting, and other essential elements for medical practice. Furthermore, with the help of high-quality multimedia, you will enhance your technical skills as you solve various real-life issues presented in each lesson.







